Key Takeaways:
- Bladder control is a complex process that involves the brain, the spinal cord, and the muscle of the bladder.
- Bowel control is similar to the bladder system, but involves the intestines, colon, and rectum instead.
- Understanding bladder and bowel control can help identify potential issues that could cause incontinence and it is important to seek help from professionals if needed.
Understanding your body is empowering and helpful in promoting healthy living. One essential aspect many people overlook is bladder and bowel control. Tonight, let us break down the complex mechanics, clarifying how these systems function, and highlighting why understanding them is crucial for overall health.
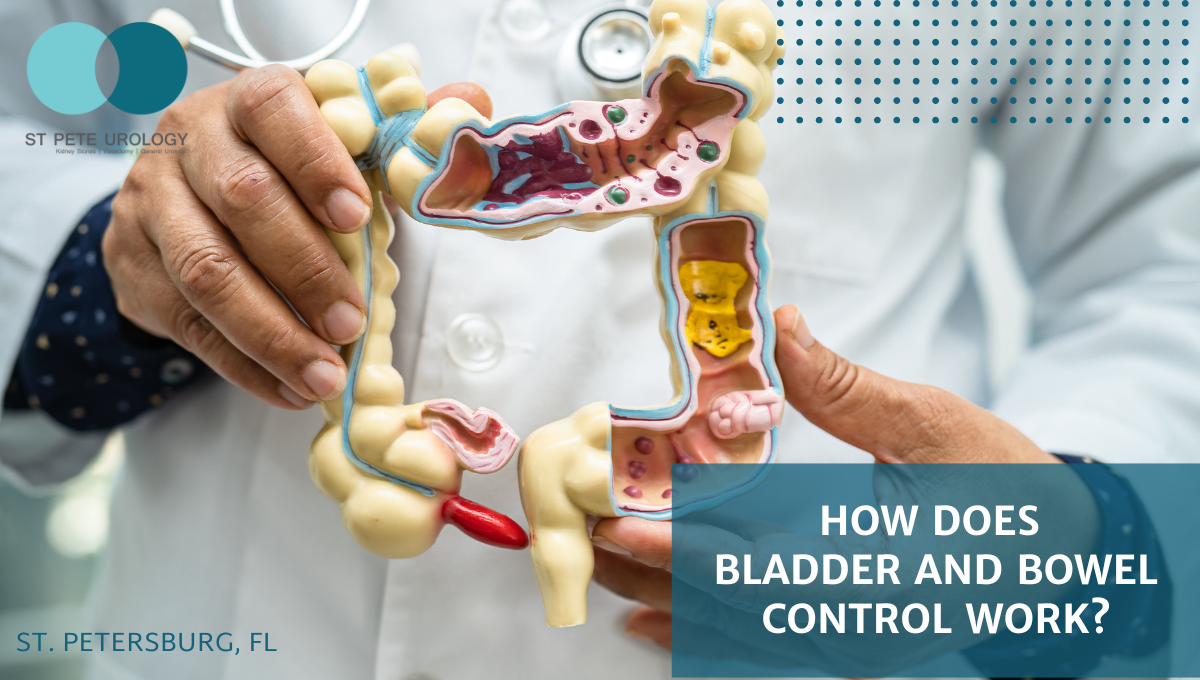
Bladder Control Mechanism


To quote Dr. Laryngakis: “Your kidneys filter your blood and make urine, and then it goes into the bladder where it’s stored, and then you pee that out. You’re supposed to be able to control that, and the bladder’s a muscle.” Acknowledging this process aids in understanding the pathophysiology of bladder control.
The bladder system is more complex than it may initially appear. As Dr. Laryngakis explains, “the bladder gets full, basically it’ll send a signal and you’ll get relaxation of the external sphincter, which is a sphincter control to control the urine, and then allow the sphincter to open, and then the bladder squeezes down and drains the bladder.” This process requires the brain’s ability to inhibit the urge to urinate and control the relaxation of the sphincter, as well as the spinal cord.
Bowel Control Mechanism
The mechanisms behind bowel control are equally intriguing. It’s rather akin to the bladder system, but instead of a bladder, there are intestines, a colon, and a rectum where stool is stored. There’s a sphincter involved here too, crucial for controlling the ability to hold the stool in place. According to Dr. Laryngakis, “that involves the brain, the spinal cord, and the muscle of the rectum and the colon involved for bowel control.”
The Importance of Understanding Bladder and Bowel Control
Recognizing the intricacies within these systems can help identify potential problems that could cause incontinence. It’s important to note that “different areas of that process can have an issue that could be fixed or could be the cause of the incontinence,” as Dr. Laryngakis stated.
Knowledge is power, but when faced with unfamiliarity or the complexity of these systems, it’s important to turn to professionals. If you are located in St. Petersburg, FL, consider St Pete Urology. Their team of experienced urologists, including Dr. Nicholas Laryngakis, is committed to providing excellent urological care and understanding these systems’ nuances. They bring their expertise and passion for urology to each patient encounter, providing individualized care for various urological issues. Remember, there’s no harm in seeking help, especially when it’s about something as vital as your health.
References:
- St. Pete Urology | Urologists in St Petersburg, Florida. (2022, December 14). St Pete Urology. https://stpeteurology.com/incontinence/
- St Pete Urology. (2022, August 25). Common Bladder Control Problems. St Pete Urology. https://stpeteurology.com/common-bladder-control-problems/
- And, D. (2023, September). Symptoms & Causes of Bladder Control Problems (Urinary Incontinence). National Institute of Diabetes and Digestive and Kidney Diseases; NIDDK – National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems/symptoms-causes
- And, D. (2023, September). Bowel Control Problems (Fecal Incontinence) – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/bowel-control-problems-fecal-incontinence
- Bowel incontinence. (2020). NHSinform.scot. https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/bowel-incontinence