What are the benefits of the PSA test?
Early detection of certain types of prostate cancer is critical for successful treatment and recovery. When the PSA test shows elevated levels of the antigen in blood, it may help to identify prostate cancer that is likely to grow quickly or spread to other parts of the body. In turn, the test helps to catch and treat such cancers early before they begin causing serious symptoms or become life-threatening. Also, by enabling early detection of prostate cancer when the necessary treatment is less aggressive, the test reduces the risk of certain adverse effects of treatment, such as urinary incontinence and erectile dysfunction.
What are the risks associated with the PSA test?
Carrying out the test itself comes with very little risk. It requires only a simple drawing of blood used to run the test in a laboratory. However, once the results of the test are out, there are a number of potential downsides involved. For instance, since false positives are quite common and elevated PSA results may have other causes other than prostate cancer, including prostate infection (prostatitis) and enlarged prostate (BPH), the test results may expose some patients to unnecessary or inappropriate treatments.
Some types of prostate cancer don’t produce much PSA, which means that a test may incorrectly indicate that you don’t have the cancer (a false negative). And follow-up tests for checking out the underlying causes of an elevated PSA test are often stressful, invasive, time-consuming or expensive. Furthermore, living with a localized or slow-growing prostate cancer — one that doesn’t require treatment — can cause stress and anxiety.
When should you get your first PSA test?
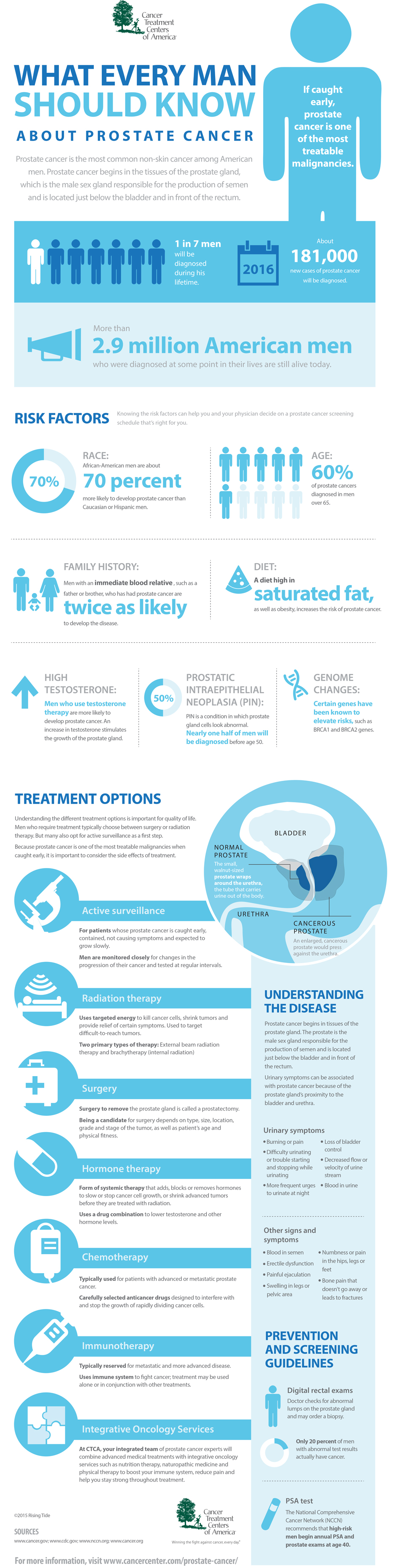
Before you get the first PSA test, it is recommended that you discuss the benefits and risks of the test with your doctor. During the discussion, a comprehensive review of your risk factors and preferences is done. For example, the urologist will consider your age, race, size of your prostate, medications you are taking (dutasteride and finasteride affect PSA levels), and how frequently your PSA levels change when making a decision about getting the test.
At St. Pete Urology, we advise men who are at higher risk of the disease, such as African American men and those with a brother or father who have had the cancer, to get their first test at the age of 40-45. Having the test before you reach 50 helps us to establish your PSA baseline and thereafter monitor the changes in your PSA levels to determine whether or not you’ll need annual PSA screening and prostate biopsy. If your blood PSA level is very low, we’ll put off any further PSA tests. But if you are a man of moderate to low risk of the disease, we recommend you get your first PSA test at age 50 or older (generally between 55 and 70).
What happens if your first PSA test result is high?
If you don’t have symptoms of prostate cancer, another PSA test may be recommended if your first test showed an elevated PSA level. The second test is used to confirm the validity of the original finding. But if the second PSA test still gives elevated PSA level, the urologist may direct that you continue with more PSA blood tests and digital rectal exams (DREs) at frequent intervals to monitor any changes in your prostate over time.
If your blood PSA level continues to rise over time or the urologist finds a suspicious lump in your prostate during a DRE, additional tests may be suggested to establish the nature of the problem. For example, a urine test may be run to find out if you have a UTI (urinary tract infection). Imaging tests like X-rays, cystoscopy or transrectal ultrasound also may be recommended. Then if prostate cancer is suspected, the urologist carries out a prostate biopsy — collecting multiple samples of tissue from your prostate by inserting hollow needles into the gland and withdrawing tissue. The tissues are examined under a microscope by a pathologist to confirm the cancer.
Treatment of prostate cancer
The type of treatment recommended for prostate cancer usually depends on whether it is early-stage or advanced-stage disease. For early-stage cancer the options include watchful waiting, radical prostatectomy, brachytherapy, conformal radiotherapy and intensity-modulated radiation therapy. At St Pete Urology, watchful waiting means no immediate treatment is offered but the cancer is closely monitored through regular PSA tests. Prostatectomy involves surgically removing part of or the entire prostate; brachytherapy involves implantation of radioactive seeds into the prostate to deliver specific amounts of radiation to the tumor. Conformal and intensity modulated radiotherapies deliver targeted amounts of radiation to the tumor with minimal damage or exposure of healthy tissues.
For advanced-stage prostate cancer, which is typically a more aggressive tumor that grows quickly and spreads faster to other areas of the body, treatment includes chemotherapy and androgen deprivation therapy. Chemotherapy can eliminate cancer cells that have spread to other parts of the body. Likewise, androgen deprivation therapy (androgen suppression therapy or ADT) is used to reduce the effect of androgens — male hormones that stimulate cancer growth — thereby slowing down or stopping cancer growth.
At St Pete Urology, we talk to our patients openly and candidly about the risks and benefits of the PSA test before we can advise them to get it. We also discuss the results of the tests, give our recommendations for those with positive results and typically repeat the PSA test for those with negative results. Our patients have always told us that our attention to detail, quality of interactions and efficiency during their visits is unmatched. If you would like to know more about the PSA test, visit the “St Pete Urology” site.