You are married and got the number of kids you always wanted. You also have decided that your family is now complete, right? So, a vasectomy it is, then. For you know that three months after a vasectomy, you will be almost 100 percent sure of no pregnancy. And that it is reversible, with 40-90 percent success rate. That’s great. Now you can go for it and enjoy wonderful times together thereafter with your spouse — no more kids to worry about.
Ready to go?
Well, yes. But there is a problem. You don’t know what it feels like to have a vasectomy and that worries you. Will it hurt? What if something goes awfully wrong down there? How long will it take to get back to 100 percent? The Internet provides answers, but you can’t tell which answers are correct. You find several men saying the experience was so easy that they were able to run a marathon the day after. But others are complaining that their experience made them feel less of a man.
Learning from others
Both sound too extreme. You want to clear the gray areas; you want true, non-medical real-talk. You want to hear from a man who has had a vasectomy and can understand your concerns. Let’s talk about what you will experience, or rather what I experienced.
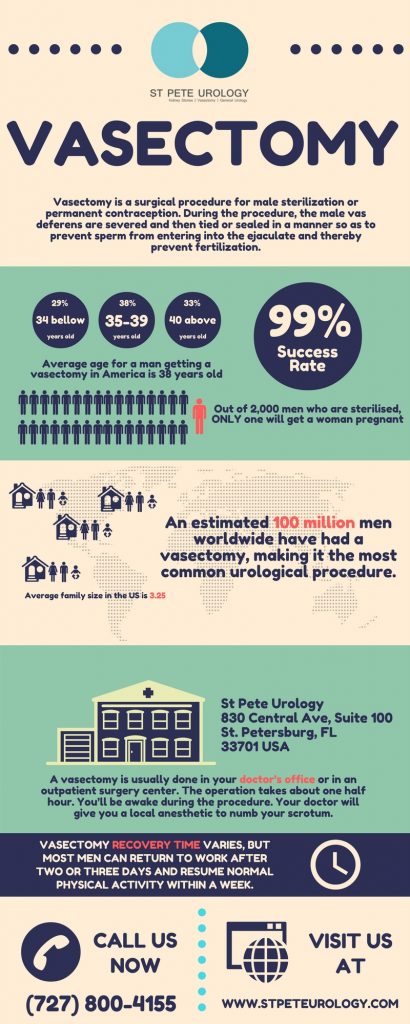
What is a vasectomy?
A vasectomy is a method of birth control that prevents pregnancy by stopping the supply of sperm to your semen. The tubes (vas deferens) carrying sperm from the epididymis to your ejaculatory ducts are sealed to prevent sperm from moving and getting into the semen. So you continue to ejaculate semen that doesn’t contain sperm and can’t cause pregnancy.
How is a vasectomy done?
Your doctor cuts open your scrotum to access the testicles (two balls inside your scrotum) and locate the tubes (vas deferens). Starting with one testicle, the urologist removes a tube, cuts a chunk out of it, closes the cut ends, puts the now-two tubes back into the testicle and stitches it shut. After that, the doctor turns to the other testicle and repeats the process. The entire procedure takes 10-30 minutes and you are free to go home. While you remain awake throughout the procedure, a local anesthetic applied to your scrotum makes sure you are numb down there. So you can engage in a chat with your doctor as the procedure goes on.
Does it hurt?
Yes, but not as much as you imagine. Initially, pain occurs when the anesthetic is applied. As the anesthetic is applied, you will feel as if someone is whacking your balls with a rubber band many times, resulting in deep, nauseating discomfort. But after that, everything down there becomes numb, though you may still feel the tugging, pulling and pressure during the procedure.
Can it go wrong down there?
Like any surgical procedure, a vasectomy comes with risks, such as infection and hematoma (bleeding in your balls). But overall, it is a safe and effective procedure. Your doctor will discuss with you all the risks of the procedure before you agree to it. And you will sign a waiver document for risks such as impotence, heart attack, bleed out, stroke and death. If you are worried that a vasectomy will trigger prostate cancer, this is the time to chat about it with your urologist. Of course studies have shown that there is no link between prostate cancer and vasectomy.
What about anxiety?
Anxiety can be a terrible part of a vasectomy. But many urologists prescribe medications to relieve anxiety, commonly a single Xanax prescription. If your doctor gives you this, don’t hesitate to take it. It will help you drift away mentally and relax, ensuring you are free from anxiety during the procedure. My urologist did not give me any such medication and I must confess that anxiety was the worst part of my experience.
What of post-op pain?
For a few days after the procedure, you have a dull, generalized soreness down there, accompanied by some low-grade stomachaches. With prescribed pain medication, you feel okay. I took Tylenol regularly plus rest and a couple of beers and felt fine. But the most serious post-op pain occurs when you catch one of the stitches with your underwear. It really hurts. I fell down like a potato sack, and believe you will too. Make sure you don’t catch one of these stitches.
How long will it take for you to recover 100 percent?
It’s different for each person. The doctor will tell you something like 10-14 days, but it may be longer or shorter for you. You definitely should keep off your feet for the first 24-48 hours and keep yourself on ice. You can start to shower after 48 hours, but that won’t be fun. I was able to walk around with slight problems after a couple of days, and started running again after a week with little soreness. I was able to resume my normal activities by day three, but that was because I felt pain-free and was quite bored after two days. Monitor your body well for pain and other complications before you get back to normal activities.
When can you begin to have sex?
The invasive stitches on your balls will remain tender and physically strange for a couple of days. This will make you quite anxious and less prepared for sex. My doctor said, “Go for sex when you are ready.” For me that was around 10 days after the procedure. Your case could be different. So don’t worry too much about it because you will get back to your old self pretty quickly once you and your spouse begin to ignite the flames of passion in the bedroom.
Where can you undergo the procedure?
Depends on which city you live in. But you should go for a doctor with years of experience performing the procedure. A place offering no-scalpel, open-ended vasectomy is great. Mine was done at St Pete Urology and it was great. The urologist was frank and friendly, and we explored a lot of questions before the procedure. Want more information on safe vasectomy? Visit the “St Pete Urology” site.