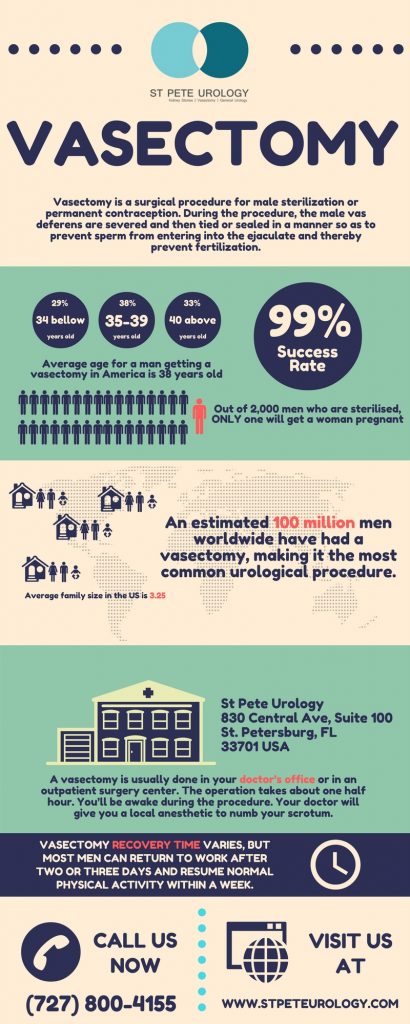
Success rate of vasectomy reversal
The success rate of reconnecting the tubes severed during vasectomy is quite high, about 90 percent. After a successful reconnection of each tube, sperm is again able to pass from the testicles through the tubes and reach semen, and a man may again be able to get his partner pregnant. But the success of a vasectomy depends on a number of factors, such as the state of the tubes during the reversal and how many years have elapsed since the vasectomy was done.
If you undergo a vasectomy reversal within seven years of the vasectomy, the reversal is a simple procedure of putting the vas deferens back together. But if the tubes are too short to reconnect, if there is scarring or it’s been more than seven years since you had the vasectomy, the reversal process may be more complex. However, even with the more complex procedure, the success rate is still around 50-60 percent with no much difference in pregnancy rates — the average being 50-60 percent likelihood of pregnancy, which drops to 44 percent if time since a vasectomy is greater than 15 years.
If the time since vasectomy is less than 15 years, the reversal provides a pregnancy rate that’s higher than in vitro fertilization (IVF) and sperm aspiration with intra-cytoplasmic sperm injection (ICSI). And even after intervals greater than 15 years since a vasectomy, the reversal still gives outcomes equal or greater than IVF with ICSI.
Vasectomy reversal techniques
Vasectomy reversal is usually performed in two ways. The first technique is vasovasostomy (VV), which is basically the piecing back together of the two sides of the tubes (vas deferens) — that is vas deferens to vas deferens. The other technique is vasoepididymostomy (VE), which involves reconnecting the vas deferens to epididymis, the duct that transports sperm to the vas deferens. Generally vasovasostomy (VV) is done if sperm is present in the vas fluid. If sperm isn’t present in the fluid, vasoepididymostomy (VE) is the go-to procedure. In some cases, a combination of both techniques may be necessary, with a vasoepididymostomy done on one side and a vasovasostomy on the other.
A vasoepididymostomy is slightly more complicated and therefore chosen only when a vasovasostomy is impossible or can’t work. You won’t know the technique that the surgeon will use until the operation begins and that usually depends on whether sperm is present in the fluid found in the vas deferens at the time of surgery. Both are outpatient procedures that take less than 3 hours. A man has a successful vasectomy reversal if sperm evaluations performed several months later indicate he has the normal sperm count necessary for conception.
How should you prepare for a vasectomy reversal?
A vasectomy reversal is a complex and expensive procedure that’s often not covered by insurance. So you should find out what you’ll need and all the costs well ahead of time. The procedure is generally more successful when performed by surgeons who are trained and experienced in microsurgical techniques and who have done the procedure several times. So when choosing a doctor for the procedure, find out how many reversals the surgeon has performed, the techniques used, how often pregnancy has occurred after surgery, and the risks and complications involved.
Similarly, you’ll need to buy tight-fitting undergarments (like an athletic supporter) that you will wear after the procedure to hold bandages in place and support your scrotum. You also will need to stop taking medications that increase the risk of bleeding, including pain relievers (like ibuprofen or aspirin) and blood-thinning drugs. You should make arrangements for your travel to and from the hospital and for the length of time you will need to recover after surgery.
What should you know before a vasectomy reversal?
Vasectomy reversal is performed as an outpatient procedure that doesn’t require an overnight stay in a hospital. Before the procedure, the surgeon will take your medical history and conduct a physical examination to make sure you’re not having any health problems that may lead to complications after or during surgery. If your physical exam shows abnormal results or you’ve got sexual function issues, the doctor may consider running some blood tests. Likewise, a review of your surgical history is done to assess whether you had any previous surgeries other than the vasectomy or prior injuries that can hinder the vasectomy reversal. The doctor also will confirm whether you can produce healthy sperm. While evidence of fathering a child before is usually sufficient proof of the health of your sperm, additional testing may be necessary if there is uncertainty.
What happens during a vasectomy reversal?
Once you’re in the operating room, anesthesia is applied to minimize discomfort during the procedure. That may either be general anesthesia to keep you unconscious throughout the procedure or a local, spinal or epidural anesthesia to minimize pain but without putting you to sleep. The surgeon then makes a small incision on the underside of your scrotum to expose the tubes (vas deferens) and free them from surrounding tissues. Cutting open the vas deferens, the surgeon examines the fluid inside the tubes to establish whether sperm is present. If it’s found that sperm is present, the doctor simply reconnects the ends of the tubes to enable sperm passage. If the fluid inside the vas deferens is pasty, thick or contains partial or no sperm, that’s usually an indication that there’s a blockage of sperm flow and that vasovasostomy may not work. In that case, vasoepididymostomy is the more appropriate procedure.
What happens after the procedure?
After the procedure, the doctor applies bandages to cover the incisions. Make sure to ask your doctor when it will be OK to take the bandages off. The stitches applied should dissolve in 7-10 days. You will be required to wear tight-fitting undergarments (like athletic supporter) and apply ice to minimize swelling. The area may feel sore for many days, but the pain shouldn’t be severe and should improve within a few days to one week.
Once back at home, make sure to take it easy and avoid any activities that may move the testicles excessively or pull on the scrotum or testicles, such as heavy lifting, biking, jogging or sporting activities. For the next several weeks, wear an athletic supporter at all times, removing it only when showering. Avoid activities such as swimming and bathing for the first two days following surgery because they can make the surgery site wet. If your job requires much driving, walking or physical exertion, seek your doctor’s advice on when it’s safe to return to work. But for a desk job, you can return to work within a few days after surgery — only making sure that nothing harms the surgery site. Do not ejaculate or engage in sexual intercourse until your doctor gives you a go ahead — that is often 2-3 weeks after surgery.
What results should you expect?
To assess the success of a vasectomy reversal, the doctor will examine your semen 6-8 weeks after surgery. If the procedure is successful, sperm will be present in the semen. The appearance of sperm in semen should happen within a few months, but may take a year or more in some cases. So the doctor may have to conduct periodic semen analysis to evaluate the success of the procedure, unless your partner gets pregnant soon after the reversal. The prospect of achieving pregnancy usually depends on a number of factors, including the age of your female partner and the duration of time that has elapsed since the vasectomy.
Can the reversal fail to work?
If a blockage develops in the tubes after surgery or there is an underlying issue with your testicles that wasn’t recognized during surgery, a vasectomy reversal can fail to work and you may need a second-attempt reversal procedure. Doctors often opt to collect and freeze some sperm during a vasectomy reversal, which can then be used if the procedure doesn’t work. But if sperm isn’t frozen during the procedure or you completely lack sperm in your ejaculate, sperm can still be retrieved directly from your epididymis or testicle to help you have children via assisted reproductive techniques, like in vitro fertilization.
At St Pete Urology, we have a huge pool of urologists trained in andrology and experienced in microsurgical techniques. We conduct the procedure under very high-level magnification using incredibly small sutures. We perform several vasectomy reversals every year and boast significantly high success rates. So if you are looking for specially trained and skilled doctors to reverse a vasectomy in a way that will maximize your chances of having children, come and see one of our urologists. For more information on vasectomy and vasectomy reversal procedures, visit the “St Pete Urology” site.