 Men, we all desire to be good husbands and partners. Many of you may have seen your wife or partner experience the adverse effects of some contraception. Some will want to help alleviate this unfortunate circumstance.
Men, we all desire to be good husbands and partners. Many of you may have seen your wife or partner experience the adverse effects of some contraception. Some will want to help alleviate this unfortunate circumstance.
The option of undergoing vasectomy may come up. This procedure is one big step to take a lead role in family planning and protect your partner. However, you may also have concerns about how it will affect your sex life afterward.
The good news is, vasectomy will not adversely affect your sex life.
It will neither reduce your sex drive nor affect your ability to have an erection. It will not affect your ability to ejaculate or have any difference in the amount of semen you ejaculate.
No effect on testosterone production
Your male characteristics depend on the hormone testosterone. Produced in your testicles and responsible for secondary sexual characteristics, testosterone is the hormone that maintains your libido (sex drive), sensation, and ability to have an erection and an orgasm.
An average testosterone level after vasectomy means you maintain the same level of sexual performance and satisfaction after the procedure.
So does a vasectomy affect your testosterone level? No. Your testicles continue to produce testosterone after the procedure, just as they did before the surgery. The operation is done on the vas deferens and not on your testicles, which means there are no effects on testosterone production. Plus, it means you continue to have normal erections, ejaculations, and orgasms.
If you experience a drop in testosterone after vasectomy, the reduction may be unrelated to the procedure. Such a reduction is often due to diminished function of the testes (hypogonadism), which is linked to age.
Hypogonadism affects 1 in 50 men aged 40-79 years. It is more common in men with diabetes, kidney disease, heart disease, or those taking certain medications, such as steroids. It may also be due to stress, depression, or too much alcohol.
If you notice any drop in your sex drive after vasectomy or feel you might have symptoms of low testosterone, speak with your doctor for help.
Normal ejaculations
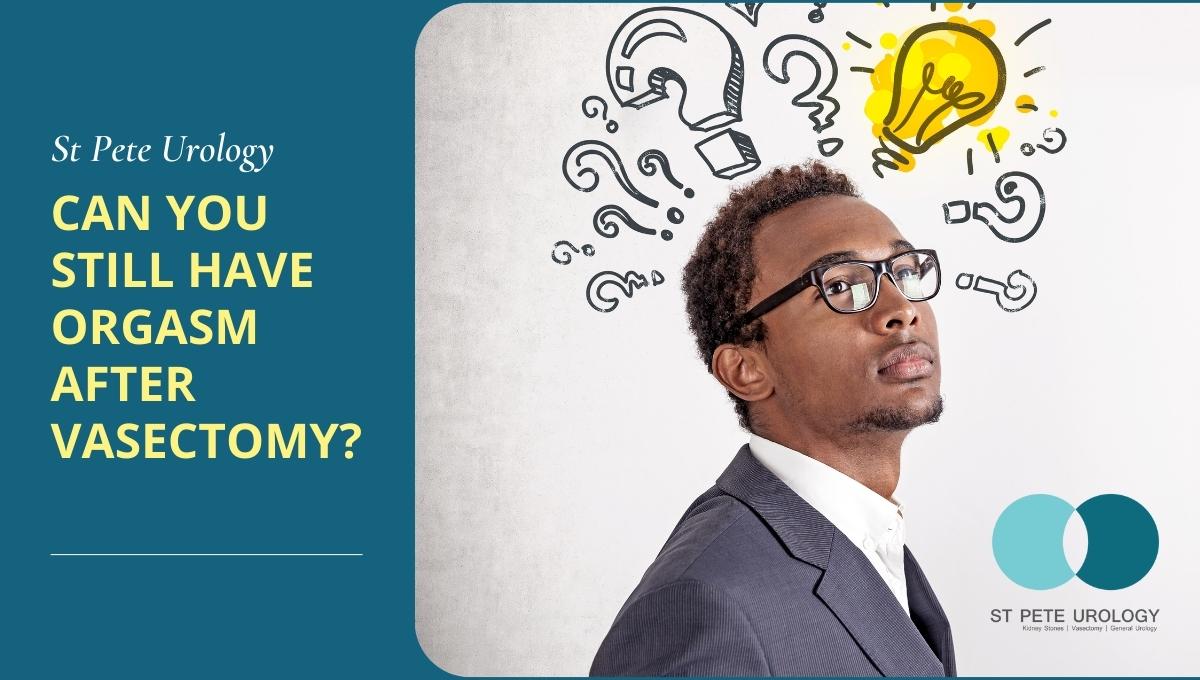
A vasectomy does not significantly affect the quantity of the ejaculate. While the procedure ensures that the sperm made in the testicles do not pass through the vas deferens to reach the urethra, it doesn’t noticeably change the quantity of fluid you ejaculate.
In a typical ejaculation, the semen produced in your seminal vesicles and prostate gland forms 95-98 percent of the ejaculate. And so, since sperm only makes 2-5 percent of the ejaculate, preventing sperm from being included in the semen doesn’t make a big difference in the volume of the ejaculate. You will not even realize the difference in your ejaculations.
Remember that the procedure does not stop sperm production. Your testicles will continue to secrete sperm throughout your life; only that the sperm will not reach the urethra to be added to the semen before ejaculation.
During a vasectomy, your vas deferens is cut and blocked to stop sperm and make it impossible for them to travel to the urethra. The sperm dies and is absorbed by the lining (membrane) of the epididymis, where they dissolve naturally. The absorption process doesn’t interfere with testosterone production, erections, or orgasms.
Enhanced orgasms
With a vasectomy, you will feel relieved from the anxiety or stress of an unplanned pregnancy. And, with that freedom, your lovemaking will be more spontaneous, sensual, frequent, and intense.
Recent studies have shown that the procedure isn’t only reliable but boosts sex drive in men and ensures stronger erections and better orgasms without the risk of pregnancy.
Safe, effective vasectomy
Want to have a vasectomy but have questions before the procedure?
At St Pete Urology, we do vasectomies every week and guide men to make the right family planning decisions. We will listen to your concerns, give you the right advice, and help you make an informed decision.
Over the years, we have seen our clients undergo vasectomy procedures and report results that make us proud. We are happy that our patients retain the highest level of sex drive, firmer erections, unchanged ejaculation, and regular orgasms after the procedure.
If you’re considering having a vasectomy at St Pete Urology, you shouldn’t fear it would affect your sex drive or orgasms. We can guarantee that your sexual performance and satisfaction will only get better.


 Urinary incontinence is a frustrating, embarrassing condition. Who wants to always be on the lookout for the nearest restroom, or have to deal with an unexpected leak during a cough, sneeze or lifting a weight.
Urinary incontinence is a frustrating, embarrassing condition. Who wants to always be on the lookout for the nearest restroom, or have to deal with an unexpected leak during a cough, sneeze or lifting a weight.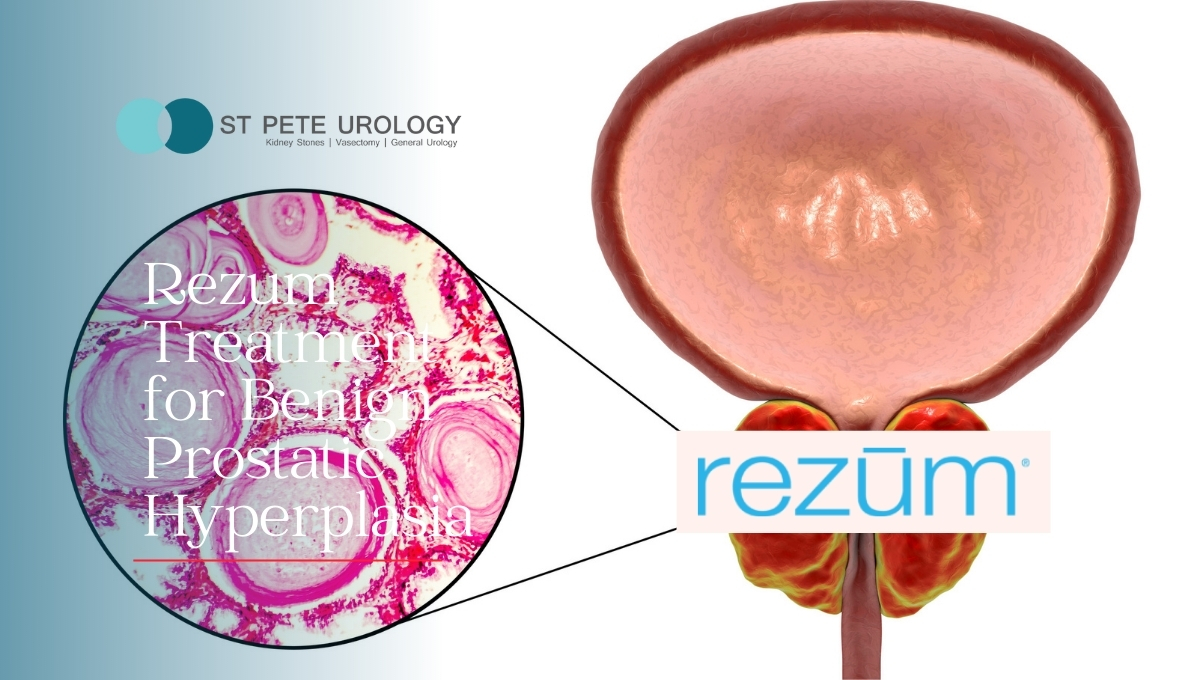
 There is no such thing as “normal” when it comes to sex. What you like isn’t necessarily what another person likes. How important it is to you and how often you want it is also a personal preference, but what is common for everyone is the desire to have a pleasurable sexual encounter.
There is no such thing as “normal” when it comes to sex. What you like isn’t necessarily what another person likes. How important it is to you and how often you want it is also a personal preference, but what is common for everyone is the desire to have a pleasurable sexual encounter.

 The occasional inability to have an erection that is firm enough for sexual intercourse is normal. However, when the problem persists for a while, it points to a deeper issue that should be addressed immediately. Without treatment, ED can make sexual intercourse impossible.
The occasional inability to have an erection that is firm enough for sexual intercourse is normal. However, when the problem persists for a while, it points to a deeper issue that should be addressed immediately. Without treatment, ED can make sexual intercourse impossible.
 Kidneys play a significant role in the overall health of the body. They filter out waste products from blood and send them out of the body as waste through urine. The kidneys also balance fluid and electrolyte levels in the body while making hormones that regulate the function of other organs of your body. But to keep your kidneys healthy, you need to watch what you eat and drink because some foods boost the performance of the kidneys while others stress, degrade and damage them.
Kidneys play a significant role in the overall health of the body. They filter out waste products from blood and send them out of the body as waste through urine. The kidneys also balance fluid and electrolyte levels in the body while making hormones that regulate the function of other organs of your body. But to keep your kidneys healthy, you need to watch what you eat and drink because some foods boost the performance of the kidneys while others stress, degrade and damage them.
 Overactive bladder (OAB) is an uncomfortable and stressful condition. Characterized by a sudden involuntary bladder contraction that triggers a compelling urge to pass urine, OAB may lead to urine leakage or the need to pass urine several times during the day or night. As a result, having an overactive bladder makes it difficult to go through the day without several visits to the bathroom.
Overactive bladder (OAB) is an uncomfortable and stressful condition. Characterized by a sudden involuntary bladder contraction that triggers a compelling urge to pass urine, OAB may lead to urine leakage or the need to pass urine several times during the day or night. As a result, having an overactive bladder makes it difficult to go through the day without several visits to the bathroom.
 Low sperm count, which means having fewer than normal sperm in the ejaculate, decreases the likelihood that your sperm will fertilize your partner’s ovum and result in pregnancy. But it may also be related to your overall health, as it is often characterized by symptoms such as pain, swelling or a
Low sperm count, which means having fewer than normal sperm in the ejaculate, decreases the likelihood that your sperm will fertilize your partner’s ovum and result in pregnancy. But it may also be related to your overall health, as it is often characterized by symptoms such as pain, swelling or a 
 Kegel exercises are for strengthening pelvic floor muscles. They involve contracting and relaxing, clenching and releasing those muscles. Also called pelvic floor exercises, Kegels strengthen and coordinate the muscles that support the bladder, rectum, uterus and small intestines. The strengthening, in turn, helps to prevent the accidental passing of stool or gas, stops bladder leaks, and improves orgasm.
Kegel exercises are for strengthening pelvic floor muscles. They involve contracting and relaxing, clenching and releasing those muscles. Also called pelvic floor exercises, Kegels strengthen and coordinate the muscles that support the bladder, rectum, uterus and small intestines. The strengthening, in turn, helps to prevent the accidental passing of stool or gas, stops bladder leaks, and improves orgasm.