A minimally invasive procedure designed to shrink prostate tissue with a series of nine-second blasts of steam offers men a new treatment for urinary symptoms commonly associated with enlarged prostates.
The procedure, called Rezūm (pronounced “resume”) and developed by NxThera Inc. of Maple Grove, Minn., became widely available in the U.S. in the second half of 2016. Thermal energy in the form of steam is applied to the prostate with a needle. As it cools it releases heat energy into the tissue, killing cells and shrinking the prostate overall by about a third, says Bob Paulson, NxThera’s chief executive.
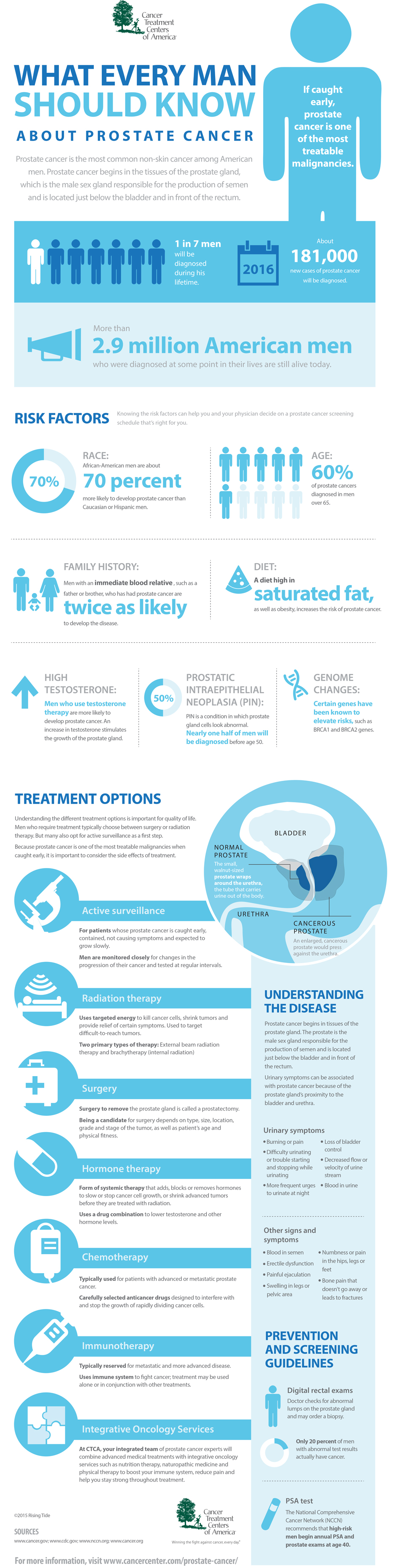
Some 50% of men over the age of 50 have enlarged prostates, which can produce symptoms such as increased urgency to urinate during the day and frequent urination, which disrupts sleep at night. Sufferers often must choose between surgery or medication, both of which have side effects, including sexual dysfunction.
The NxThera therapy is the second major innovation in recent years for men with enlarged prostates. The other, an implanted device called UroLift, was introduced in the U.S. in 2013 by NeoTract Inc. of Pleasanton, Calif.
After years of little improvement in the minimally invasive treatment of enlarged prostates, men now have two new options “that leave your sexual function intact,” says Claus G. Roehrborn, a professor and chairman of the department of urology at the University of Texas Southwestern Medical Center in Dallas and a co-author of published studies on both treatments.
Middle ground
Physicians say Rezūm can be used on a wider range of prostate anatomies than the UroLift implant. The procedure, which costs about $2,000 and generally is covered by insurance, can be done in a doctor’s office in just a few minutes. To dull pain, lidocaine may be injected into the prostate, and most doctors will offer a sedative for patients who want one. After the procedure, most patients need to wear a catheter for two or three days but can return to daily activities immediately.
While the results of a two-year clinical trial published by Dr. Roehrborn and colleagues show that Rezūm provides significant relief from symptoms, it isn’t clear how long the improvement will last.
“The durability issue is what’s going to sink or swim this procedure,” says study co-author Kevin T. McVary, chairman and professor of urology at Southern Illinois University School of Medicine, in Springfield, Ill. Both minimally invasive options are likely less effective than surgery, Dr. Roehrborn says, because surgery removes the most tissue.
Still, for many men, the steam treatment offers an appealing middle ground between the risk of surgery and the hassle and side effects of taking daily medication, which can cause dizziness and fatigue.
“I tried Flomax for about two years but the side effects were too annoying,” says Stephen Gooding, a 60-year-old utility supervisor from Grayson, Ga., who says the drug made him dizzy and constipated. He had the Rezūm procedure in October, and now “I feel like I did 30 years ago.”
In the two-year study of 197 men, funded by NxThera and published online in the Journal of Urology in December, patients who had the Rezūm procedure showed a significantly greater improvement in symptoms at three months compared with patients who had a sham procedure. At the end of two years, patients treated with Rezūm showed a 51% reduction in urinary symptoms (as measured by a seven-question survey), compared with the beginning of the study.
Over the two years, about 4% of the patients who underwent Rezūm had to have a repeat procedure or surgery to treat their condition. Early in the trial, physicians were new at performing the procedure and didn’t always remove enough tissue, says Cindy Ogden, vice president, clinical affairs at NxThera.
So far, Rezūm appears to spare men sexual side effects. In the surgical procedure known as transurethral resection, 70% to 80% of men generally get a condition called retrograde ejaculation, also called dry orgasm, says Dr. McVary.
In the Rezūm study, about 3% of the patients who underwent the procedure experienced no ejaculatory volume afterward, and 5.3% experienced a decrease in ejaculatory volume, according to data provided by NxThera. Ejaculatory volume can fluctuate over time in men with enlarged prostates, so it isn’t clear the reductions were caused by the procedure, Dr. McVary says. Overall in the study, there was no average change in ejaculatory volume, he adds.
Larger prostates
A major advantage of Rezūm is that it can be done on most types of anatomies. UroLift isn’t approved by the Food and Drug Administration to treat the median, or middle lobe of the prostate, which contributes to symptoms in about 10% to 30% of patients, Dr. Roehrborn says.
The FDA hasn’t cleared Rezūm or UroLift for prostates weighing more than 80 grams. So NxThera can’t market its procedure for larger prostates, though doctors can legally use it on such patients if they choose.
Early results in clinical practice on large prostates appear “promising” and a study on prostates up to 150 grams is expected to begin later this year, says Ricardo Gonzalez, a urologist at Texas Medical Center in Houston, who will be a principal investigator on the research. About a quarter of men seeking treatment for prostate-related urinary symptoms have prostates greater than 80 grams, he says.
Business executive Jim Bracke, 69, says that, with just a Tylenol and the lidocaine shot, discomfort from Rezūm’s steam blasts felt no more intense than “warm water spilled on the groin.” He drove himself home after the procedure, and says he’s thrilled that he no longer needs to check out a bathroom the moment he arrives at a restaurant. And as long as he doesn’t overdo it, he adds, “I can have beer, and coffee and chocolate and still sleep through the night.”