It is a common mistake to believe that only men see urologists. In fact, women are more likely than men to have a urinary problem at some stage of life. When it comes to a condition affecting the urinary tract, bladder or kidneys, a urologist is the expert who can offer the best treatment. Urologists see women, men and children to treat common disorders of the urinary system.
Women’s Urological Conditions
(a) Overactive bladder: A woman with an overactive bladder experiences a sudden, frequent or hard-to-control urge to urinate, wakes up more than once at night to urinate, or urinates eight or more times in 24 hours. A urologist will perform various tests to diagnose the disorder and then recommend treatment according to the cause.
(b) Urinary incontinence: Characterized by a loss of bladder control that often results in accidental leakage of urine, urinary incontinence affects up to 57% of women between 40-60 years and requires the attention of a urologist.
(c) Urinary tract infections (UTIs): Urinary tract infections can cause serious complications if they spread to the kidney. They require prompt and effective treatment. Since women are more susceptible than men to UTIs because of their anatomy, they should see a urologist if they have frequent or persistent infections.
(d) Fallen bladder: Because the bladder is held in position by the pelvic floor, it may drop onto the vagina when the pelvic floor is weakened or stretched due to obesity, menopause, aging or prior pelvic surgery. A woman should see a urologist with experience in female urology to correct a fallen bladder.
(e) Painful bladder syndrome (interstitial cystitis): Interstitial cystitis (IC) comes with lower belly and bladder discomfort, a feeling that the bladder is always full, and a sudden and severe urge to urinate (even up to 60 times per day), which can interfere with everyday activities. Some women have been forced to skip social events or avoid travelling away from home, while some find sex uncomfortable or painful due to the condition. Women who have the disorder need to see a urologist.
(f) Urinary stones: Urinary stones are hard masses that form in the kidneys, bladder or ureters. While drinking 2-4 quarts of water in 24 hours may help to move a urinary stone, a urologist can break them apart with ultrasound-based treatment or remove them surgically.
(g) Cancer: Women can have cancer in the bladder, bladder lining, kidneys or urethra. The cancer may show signs such as pain during urination, lower back pain, blood in urine and frequent visits to the bathroom. Seeing a urologist may help to detect and treat the cancer early.
Ideally, women should see a urologist when experiencing:
- Pelvic pain
- Burning sensation or discomfort when urinating.
- Frequent urination
- Blood in urine
- Pain in the back or sides
- Leaking urine
At St Pete Urology, we have specialized urology services that cater to the unique needs of women. We deal with many urological conditions affecting women, including incontinence, pelvic organ prolapse, bladder infection, overactive bladder, kidney stones and cancer. Male or female, feel free to contact St Pete Urology when you have a urine or bladder issue.


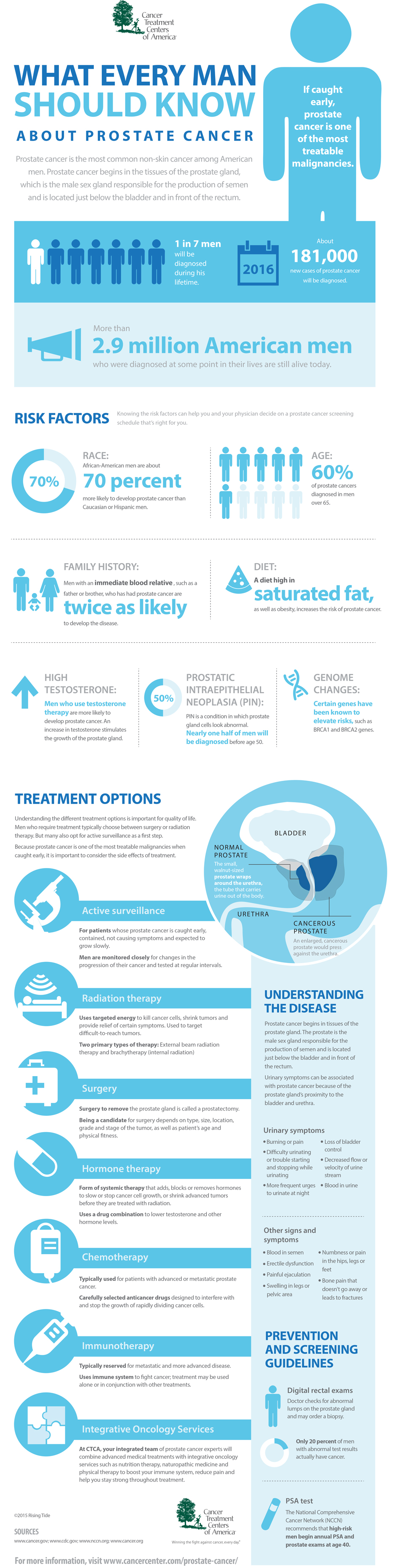
 Also called Image Guided Radiation Therapy (IGRT), this form of treatment has been implemented at St Pete Urology with great success for prostate patients. Our state-of-the-art imaging enables urologists to direct radiation with more precision to the area of the prostate that requires treatment. With better preparation and planning, this technology ensures more accuracy and allows the urologist to target the same area of the prostate for all additional treatments. In fact, EBRT ensures less radiation and pinpoint accuracy for better outcomes and reduced side effects associated with radiotherapy.
Also called Image Guided Radiation Therapy (IGRT), this form of treatment has been implemented at St Pete Urology with great success for prostate patients. Our state-of-the-art imaging enables urologists to direct radiation with more precision to the area of the prostate that requires treatment. With better preparation and planning, this technology ensures more accuracy and allows the urologist to target the same area of the prostate for all additional treatments. In fact, EBRT ensures less radiation and pinpoint accuracy for better outcomes and reduced side effects associated with radiotherapy.

 When using a prescription for managing enlarged prostate, you will take the pills every day for life, have regular medical checkups, and use special bathroom techniques such as relaxation and double voiding. The medicines will reduce the risk of urinary retention, relieve symptoms and minimize risks of future surgery. However, prescriptions are often expensive and come with certain side effects such as trouble getting an erection, diminished sex drive, tiredness, dizziness, and stuffy nose.
When using a prescription for managing enlarged prostate, you will take the pills every day for life, have regular medical checkups, and use special bathroom techniques such as relaxation and double voiding. The medicines will reduce the risk of urinary retention, relieve symptoms and minimize risks of future surgery. However, prescriptions are often expensive and come with certain side effects such as trouble getting an erection, diminished sex drive, tiredness, dizziness, and stuffy nose.