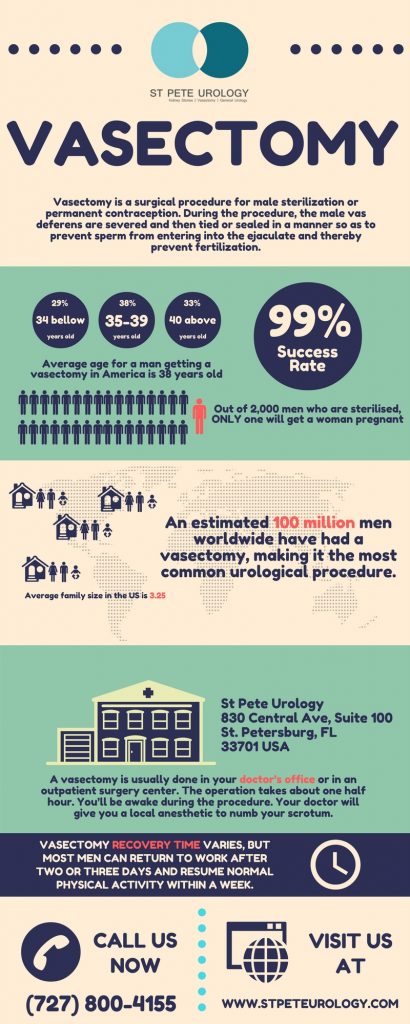
Vasectomy is considered a permanent birth control method because it prevents the release of sperm during ejaculation. During a vasectomy, the tube (vas deferens) from each testicle is carefully clamped, sealed or cut to prevent the mixing of sperm with ejaculated semen. The testicles will continue to produce sperm but the female egg cannot be fertilized without sperm in the semen. Since the tubes are sealed off before the seminal vesicles and prostate, a man will still ejaculate the same amount of fluid.
So what happens during a vasectomy?
- (a) The testicles and scrotum are first cleaned with antiseptic and may be shaved.
- (b) You may be given an intravenous (IV) or oral medicine to minimize anxiety and make you sleepy. If given the medicine, you may not remember much of what happens during the procedure.
- (c) The urologist will locate each vas deferens by touch and then inject a local anesthetic into the area.
- (d) The doctor will make 1 or 2 small openings on the scrotum. Then through an opening, the 2 vas deferens tubes are cut, tied and stitched, or sealed. Scar tissue from the operation will help block the tubes.
- (e) The urologist will then replace the vas deferens inside the scrotum and close the skin with stitches that dissolve on their own. A vasectomy procedure takes 10-30 minutes and can be done in a clinic or office of a urologist, general surgeon or family medicine doctor.
How does vasectomy work?
The scrotum will be numb for 1 to 2 hours after the surgery. You are expected to apply cold packs to the area and get as much rest as possible while lying on your back. Wearing a jockstrap or snug underwear will protect the area and ease the discomfort. You may experience minor pain and swelling for a few days, but rarely anything more serious. After two days you can resume light work, but must wait for at least a week for heavy lifting and strenuous work.
While you can resume sexual intercourse as soon as you feel comfortable, waiting for a week is advisable. Remember, your sperm count will not be zero and you can still get your partner pregnant, so use an alternative birth control method such as condoms until follow-up sperm count tests show no sperm in the semen, usually two months after the procedure.
Vasectomies are 99.85% effective, with only 1 or 2 women in 1000 getting pregnant after their partners have undergone the procedure. It will not interfere with your sex drive, sensation of orgasm, ability to ejaculate or ability to have erections. However, it is a permanent birth control method that must only be considered by those who do not want to have children in the future. For more information on vasectomies, visit St Pete Urology in St Petersburg, Florida.