Key Takeaways:
- Kidney and bladder stones are distinct entities with unique causes, symptoms, and treatments.
- Early diagnosis and appropriate treatment are critical in managing both kidney and bladder stones and minimizing their impact on overall health.
- Prevention strategies for kidney and bladder stones include staying hydrated, eating a balanced diet, and treating underlying conditions.
When discussing kidney stones and bladder stones, it’s crucial to note that while they may share similarities in composition and origin, they are distinct entities that manifest uniquely and require separate interventions. Knowing the difference can be key to understanding your symptoms and seeking appropriate treatment.
Causes and Risk Factors
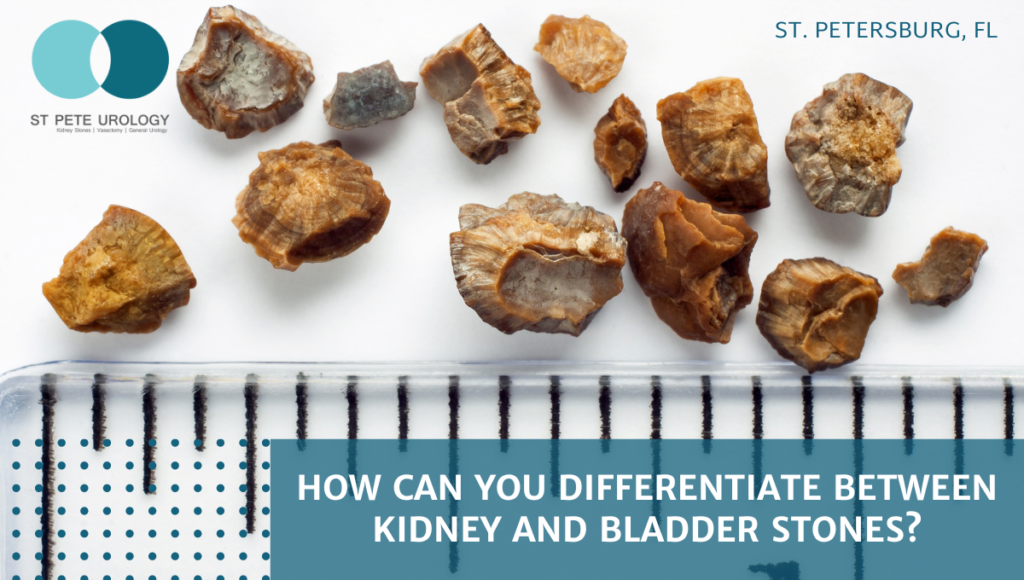
- Kidney stones are frequently the result of accumulating crystals of calcium or uric acid, often rooted in dietary habits, dehydration, or specific medical conditions. The higher concentration of these substances in your urine, the greater the risk of formation.
- Bladder stones, on the other hand, are usually born from recurrent urinary tract infections (UTIs) or from situations that impede urine flow, such as urinary tract blockages or an enlarged prostate. They form when concentrated minerals in the urine crystallize inside the bladder.
Symptoms
Symptoms of kidney and bladder stones can vary greatly, which is why discerning between the two can be so crucial.
- Kidney stones often initially manifest as sharp, severe pain in the back or side below the ribs – a pain so intense, it’s been equated with childbirth. Blood in the urine is a telltale sign, as is an increased frequency and urgency of urination. You may also experience nausea and vomiting.
- Bladder stones differ in that they often cause a noticeable discomfort in the lower abdomen. Like kidney stones, they can increase the frequency of urination, but they may also result in difficulty starting or stopping urine flow, besides the presence of blood in urine.
Diagnostic Tools and Tests
- Diagnosing kidney stones may involve imaging tests such as CT scans, ultrasounds, or X-rays to visualize the stone.
- Bladder stones, conversely, can be diagnosed through a physical examination or similarly with an ultrasound or X-ray. In some cases, a cystoscopy, which uses a thin tube passed through the urethra, is used for diagnosis.
Treatment Options
When kidney stones are small, they may pass on their own – a process expedited by hydration and managed with pain medication. In more severe cases, medications to aid stone passage or dissolve certain stones can be used, or surgical procedures like lithotripsy or nephrolithotomy for larger stones.
Treatment of bladder stones can range from removal during a cystoscopy (for smaller stones) to surgery for larger or complex cases. Addressing underlying causes, such as urinary blockages or UTIs, is often part of the treatment plan.
Prevention Strategies
For kidney stones, staying well-hydrated and eating a balanced diet low in salt and oxalate-rich foods is key. Healthcare professionals may also prescribe particular medications for individuals at high risk.
Prevention of bladder stones often involves appropriate treatment of UTIs, regular emptying of the bladder, and managing underlying conditions, such as an enlarged prostate.
Conclusion
In differentiating kidney stones from bladder stones, it’s clear that despite their similarities, the differences in causes, symptoms, and treatments make them unique health concerns. Early diagnosis and appropriate treatment are critical in managing both and minimizing their impact on your overall health and wellbeing. If you are experiencing symptoms, seeking prompt medical attention is of utmost importance.
For those based in Florida, St Pete Urology is a practice staffed with highly experienced urologists who offer comprehensive care for bladder stones, kidney stones, and other urological conditions. Remember, when it comes to your health, subtleties matter. Swiftly assessing symptoms, seeking professional advice, and beginning an effective treatment plan sooner rather than later could make all the difference. Don’t ignore your body—listen to it and act.
References:
- St. Pete Urology | Urologists in St Petersburg, Florida. (2022, July 11). St Pete Urology. https://stpeteurology.com/kidney-stones/
- St Pete Urology. (2011, November 4). Recurring Urinary Tract Infections. St Pete Urology. https://stpeteurology.com/recurring-urinary-tract-infections/
- St Pete Urology. (2019, July 8). St. Pete Urology | Urologists in St Petersburg, Florida. St Pete Urology. https://stpeteurology.com/why-do-i-keep-getting-utis/
- Kidney Stones. (2021, December 13). National Kidney Foundation; https://www.kidney.org/atoz/content/kidneystones
- NHS Choices. (2023). Overview – Bladder stones. https://www.nhs.uk/conditions/bladder-stones/
- Imaging Tests to Check for Kidney Stones in the Emergency Department | Effective Health Care (EHC) Program. (2016). Ahrq.gov. https://effectivehealthcare.ahrq.gov/products/kidney-stone-imaging/consumer