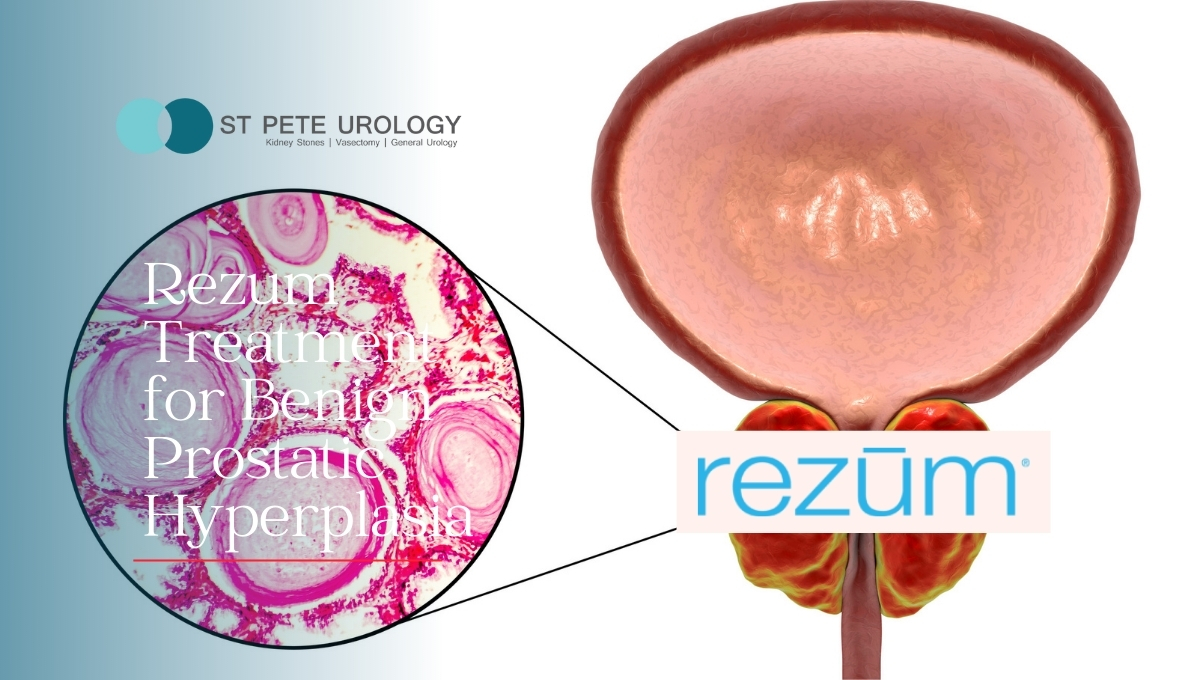
Benign prostatic hyperplasia (BPH), also called enlarged prostate, is a frustrating condition commonly occurring as men grow older.
Continue readingWhat is sex like with a penile prosthesis
ST PETE UROLOGY IS FIRST TO OFFER NEW MEDICAL TECHNOLOGY FROM MEDTRONIC TO TREAT PEOPLE SUFFERING FROM INCONTINENCE
World Continence Week 2021
Welcome to World Continence Week, June 21-27! Let’s talk about what nobody wants to talk about – leaks and accidents. Do you always leave the house with pads and fresh clothes? Constantly looking for the nearest bathroom? You are not alone! 47 million adults have OAB1 in the US today. http://controlleaks.com #WorldContinenceWeek

What is the fastest way to cure erectile dysfunction
 The occasional inability to have an erection that is firm enough for sexual intercourse is normal. However, when the problem persists for a while, it points to a deeper issue that should be addressed immediately. Without treatment, ED can make sexual intercourse impossible.
The occasional inability to have an erection that is firm enough for sexual intercourse is normal. However, when the problem persists for a while, it points to a deeper issue that should be addressed immediately. Without treatment, ED can make sexual intercourse impossible.
So what is the fastest way to cure erectile dysfunction?
1. Make lifestyle changes
If you have erectile dysfunction, you can get quick results by making a few lifestyle changes that ensure enhanced blood flow to the penis and help achieve harder erections.
For example, if you quit smoking, lose weight, or exercise regularly, you may see an improvement in your sexual function. You may also need to speak with your doctor if you suspect that a medication you are taking contributes to your ED. Your doctor may change or withdraw the medication.
2. Using oral medication
You can get quick results through oral medications such as Viagra, Cialis, Levitra, Staxyn, or Stendra. These pills boost blood flow to the penis during sexual arousal, making it possible to achieve an erection that is firm enough for satisfactory sexual intercourse.
These pills require a doctor’s prescription to guarantee safety and should not be taken more than once per day. They are taken 30-60 minutes before sexual activity. Cialis can be taken up to 36 hours before sexual activity and comes with a lower daily dose.
3. Injectable drugs
If you don’t like pills, injectable medications for ED can help you achieve a stronger erection. They are injected directly into the penis and work by widening the blood vessels, making the penis engorged with blood.
Alternatively, you can use a medicated pellet that you insert into your urethra to trigger an erection within a few minutes.
If you are considering injectable drugs as an option, please make sure to discuss the details with your urologist.
4. Vacuum devices
Also called pumps, vacuum devices provide an alternative to medication. To use the pumps, you place your penis inside a cylinder connected to the pump. The pump draws out air from the cylinder to create a partial vacuum around the penis. As a result, blood rushes into and fills your penis, causing an erection.
You will have an elastic band around the base of your penis to maintain the erection during intercourse. But if you are considering using a vacuum device, it is important to discuss its proper use with your urologist because the elastic band must be used correctly to avoid potential penile damage.
5. Penile implant surgery
If you have tried pills and other less invasive options without success, you may need to undergo penile implant surgery. This option is ideal if your penile blood vessels have been damaged by severe diabetes or during radical prostatectomy. You may also need to undergo penile implant surgery if you have structural problems that make erections difficult or impossible.
There are two basic types of penile implants: inflatable and non-inflatable. The non-inflatable (malleable) implant is a single rod that can be shaped by hand to create an erection. The inflatable implant has two rods filled with fluid from a reservoir located near the bladder.
When you desire an erection, you use the pump to fill the rods with pressurized fluid. As the rods fill, the penis becomes erect and broader. The prosthesis leaves the penis completely deflated when there is no fluid in the rods, making the penis implant unnoticeable.
Want to overcome erectile dysfunction fast?
At St Pete Urology, we offer various safe, effective treatments for erectile dysfunction, including medications, injections, vacuum devices, and penile implants.
We are proud of what we have been able to achieve for our patients. In most cases, our patients have the same level of sexual satisfaction and ability to ejaculate that they had before the erectile dysfunction.
If you have trouble with erections, speak with our skilled urologists and begin your journey to a life of renewed self-esteem, confidence, and optimum sexual function. For more information about effective treatments for erectile dysfunction, visit the St Pete Urology website.
What is the Best Procedure for Kidney Stone Removal?
 Urologists treat kidney stones based on their type, size and location. Smaller kidney stones can pass on their own without treatment. Your urologist may advise you to drink plenty of fluids to help the stone move along your urinary tract. You will be able to pass smaller stones naturally without any treatment other than pain-relieving medication.
Urologists treat kidney stones based on their type, size and location. Smaller kidney stones can pass on their own without treatment. Your urologist may advise you to drink plenty of fluids to help the stone move along your urinary tract. You will be able to pass smaller stones naturally without any treatment other than pain-relieving medication.
For kidney stones that are larger and block your urinary tract or cause unbearable pain, you may need treatment to break down and remove the stones. If you are vomiting and dehydrated, urgent treatment is necessary.
So what is the best procedure for kidney stone removal?
For larger stones causing excruciating pain or that may not pass on their own, surgery is typically the best treatment. There are four surgical procedures your urologist may consider: shockwave lithotripsy, ureteroscopy, percutaneous nephrolithotomy, and robot-assisted surgery. The best surgical procedure for your kidney stones will depend on their type and location.
You will need surgical kidney stone removal if:
- You have a lot of pain
- You have large stones that cannot pass on their own
- Your stones are blocking urine flow out of your kidneys
- You have recurrent urinary tract infections due to stones
At St Pete Urology, our urologists are highly trained and experienced in a full range of surgical procedures for removing kidney stones. We conduct minimally-invasive procedures which guarantee faster healing.
The procedure we perform on a patient will depend on the nature and location of the stone, the patient’s overall health, and other factors.
We ensure that you get the best possible care as quickly as possible, from surgery through recovery.
How are the surgical procedures performed?
1. Shock Wave Lithotripsy
Shock wave lithotripsy (SWL) is a procedure in which kidney stones are targeted using sound waves and X-rays. The stones are broken down before they are passed naturally in urine. This non-invasive procedure is used for small to medium-sized kidney stones, usually less than two centimeters in size, softer, and located in the ureter.
During the procedure, you lie on a table and receive medicine to limit pain and discomfort before high-energy shock waves are aimed at the stone from the outside. No cuts are made in your skin as the waves go through and break the stones into smaller pieces. Your urologist may insert a tube in your ureter, called a stent, which will aid in passing the stones. The procedure will take about an hour and you are free to go home the same day. Recovery time for shockwave lithotripsy is relatively short, so you will be able to return to normal activities within a few days.
2. Ureteroscopy
For bigger stones, your urologist may consider ureteroscopy. For this procedure, a small scope, called a ureteroscope, is inserted into the kidney via the bladder. When the stone is in the upper part of the ureter and kidney, your urologist will use a more flexible ureteroscope. If the stones are in the lower portion of the ureter near the bladder, a rigid scope may be used. Ureteroscopy is an outpatient procedure done without incision and under general or spinal anesthesia.
At St Pete Urology, one of the most common surgeries to treat kidney stones is ureteroscopy with Holmium laser lithotripsy. During this procedure, the urologist inserts a narrow, flexible ureteroscope through your urethral opening and passes it through the bladder to reach the stone. The stone is then collected from the location or broken up using a small laser fiber and removed.
3. Percutaneous nephrolithotomy
Percutaneous nephrolithotomy is a minimally-invasive procedure in which a surgeon makes a small incision, usually at the back or side to create a tunnel directly to the kidney to break and remove a large or irregularly shaped stone. Once an incision is made, an optical instrument, called a nephroscope, is inserted through the incision to reach the stone. The stone is broken down into small pieces and drawn out. This procedure is ideal for kidney stones that are big (larger than 2 centimeters), numerous, too dense, or located in a hard-to-reach area in the kidney or ureter. A stent is inserted to help with the excretion of urine as you heal from the surgery. You may need an overnight stay in the hospital after the procedure and can expect to recover in two to four weeks.
4. Robot-assisted stone removal
Kidney stones can also be removed using the da Vinci surgical system, particularly if you were born with a kidney drainage problem (ureteropelvic junction obstruction) or have complicated stones that cannot be removed successfully using other surgical methods.
This robotic surgical system gives urologists a high-resolution and three-dimensional view of small areas. It allows for an increased range of motion and the ability to make more precise incisions, which ensure less scarring. Patients who undergo this procedure recover more quickly and spend fewer days in the hospital, compared to those who have had traditional open surgery.
Why have your kidney stone removal at St Pete Urology?
At St Pete Urology, our urologists frequently treat patients with kidney stones of different types, locations and sizes. We perform hundreds of kidney stone surgeries every year, using mostly minimally invasive and robotic procedures.
Your condition will be managed by specialists who will recommend the best procedure, apply a personalized treatment plan, and deliver top-notch follow-up care. We will see you through your recovery period and monitor your progress to make sure you are in the best of health.
For more information on kidney stone prevention, diagnosis and treatment, visit the St Pete Urology website.
What Foods Are Good For Kidneys?
 Kidneys play a significant role in the overall health of the body. They filter out waste products from blood and send them out of the body as waste through urine. The kidneys also balance fluid and electrolyte levels in the body while making hormones that regulate the function of other organs of your body. But to keep your kidneys healthy, you need to watch what you eat and drink because some foods boost the performance of the kidneys while others stress, degrade and damage them.
Kidneys play a significant role in the overall health of the body. They filter out waste products from blood and send them out of the body as waste through urine. The kidneys also balance fluid and electrolyte levels in the body while making hormones that regulate the function of other organs of your body. But to keep your kidneys healthy, you need to watch what you eat and drink because some foods boost the performance of the kidneys while others stress, degrade and damage them.
What foods support healthy kidneys?
Kidney-friendly foods are those that enhance kidney function and protect them from damage. Generally, a good balance of quality protein, calories, vitamins, and minerals are great for the kidneys. Very high dietary levels of some mineral ions such as sodium, potassium, phosphorus and calcium may in the long run endanger your kidneys. Foods linked to heart problems and high blood pressure may put additional pressure on the kidneys.
For healthy kidneys, consider the following:
1. Stay Hydrated
Water helps to flush out toxins from the body. In fact, the body relies on water to assist transporting toxic wastes into the bloodstream, then to the kidneys where they are filtered and removed through urine. This process helps reduce the risk of bacterial infection, kidney stones, and kidney disease, which is why water is crucial for the critical salt-fluid balance in the body.
Ideally, you should drink 6-8 glasses of water per day, but of course you can drink more if you are active during the day. In addition to the many other benefits of staying hydrated, drinking water when thirsty helps to support your kidneys.
2. Apples and mushrooms
Apples are rich in fiber. One of the fibers, called pectin, helps to reduce various risk factors for kidney disease, such as high blood sugar and cholesterol levels. Apples also have anti-inflammatory constituents, prevent constipation, protect against heart disease, and lower the risk of cancer. You might also consider eating mushrooms for their high levels of vitamin D, which boosts kidney function.
3. Sweet potatoes
Sweet potatoes have a robust fiber profile. They break down very slowly in the body which helps to support low insulin levels. Sweet potatoes also have a healthy amount of vitamins and minerals, such as potassium which helps to balance sodium levels in the body and reduce the effect of sodium on the kidneys. However, since they contain high levels of potassium, sweet potatoes are not ideal for those with chronic kidney disease (CKD).
4. Berries
Dark berries, such as strawberries, raspberries and blueberries are a great source of nutrients and antioxidants and for most people protective for the kidneys.
5. Dark leafy vegetables
Leafy vegetables such as kale, spinach and chard contain a wide variety of vitamins, fibers, and minerals that support kidney function. While they do supply a number of protective compounds, dark leafy vegetables are highly rich in potassium and therefore less suitable for those with chronic kidney disease (CKD), restricted diet, or patients on dialysis.
6. Kale and cauliflowers
Kale is a terrific source of vitamins A and C which reduce inflammation, boost the immune system and protect the kidneys. Kale is also lower in potassium compared to other greens, and contains lots of iron. Like kale, cauliflower is rich in vitamin C and also has plenty of fiber and folate that are crucial for kidney function. Likewise, cauliflower contains compounds that improve the liver’s ability to neutralize toxic substances and reduce the stress on the kidneys.
7. Fatty fish and egg whites
Tuna, salmon and other cold-water, fatty fish have high omega-3 fatty acids. The omega-3 fatty acids in these fish are heart protective and also healthy for the kidneys. Since high blood pressure is a risk factor for kidney disease, fatty fish is a great way to improve your cholesterol profile and protect your kidneys.
Foods to avoid include:
1. High salt
Elevated salt levels raise blood pressure making the heart and kidneys work extremely hard. You can control your salt intake by cooking at home and avoiding most fast foods which are sky high in sodium.
You can also try substituting new spices and herbs in place of salt and by avoiding packaged and pre-cooked foods, such as soups, frozen dinners, and boxed meals that usually have extra salt. Similarly, you should avoid table salt and high-sodium seasonings like soy sauce, garlic salt and sea salt.
2. Foods rich in potassium
While potassium helps your nerves and muscles to work properly, too much of it can lead to serious heart problems and eventually to kidney issues. Potassium is found in most fruits and vegetables, such as bananas, oranges, avocadoes, raw carrots, cooked broccoli, potatoes, greens, tomatoes, and melons.
Instead of these high potassium foods, try alternatives such as apples, cranberries, blueberries, raspberries, and strawberries. Other good options are pineapples, peaches, plums, asparagus, cabbage, cucumber, and beans (green and white).
3. Limit phosphorus and calcium
Phosphorus and calcium are great minerals for keeping your bones healthy and strong. But high levels of phosphorus may increase the risk of long-term kidney disease. Since most foods that contain phosphorus are also equally rich in calcium, the body’s levels of the two minerals can be controlled by similar mechanisms.
If your doctor suggests limiting phosphorus, avoid foods such as red meat, dairy products, nuts, fish, most grains, and legumes. Consider replacing these foods with healthy foods that are lower in phosphorus, such as fresh fruits and veggies, rice, corn and fish.
At St Pete Urology, we encourage our patients to take care of their kidneys through healthy behaviors—exercise, drinking plenty of water and eating a balanced diet. We also perform surgeries and treat urination problems such as incontinence, tumors, cysts, growth and stones of the urinary system, as well as problems of the male reproductive system. For more information on kidney disorders and their treatment, visit the St Pete Urology website.
Overcoming an Overactive Bladder
 Overactive bladder (OAB) is an uncomfortable and stressful condition. Characterized by a sudden involuntary bladder contraction that triggers a compelling urge to pass urine, OAB may lead to urine leakage or the need to pass urine several times during the day or night. As a result, having an overactive bladder makes it difficult to go through the day without several visits to the bathroom.
Overactive bladder (OAB) is an uncomfortable and stressful condition. Characterized by a sudden involuntary bladder contraction that triggers a compelling urge to pass urine, OAB may lead to urine leakage or the need to pass urine several times during the day or night. As a result, having an overactive bladder makes it difficult to go through the day without several visits to the bathroom.
Bothersome Symptoms
While the symptoms of OAB may be less troublesome when you are at home, they can be a problem in a public or unfamiliar place. No one wants to rush out of meetings with important clients or friends for fear of not making it to the restroom in time.
The fear instilled by overactive bladder can interfere with your ability to go out with friends, work, exercise, and even sleep. It can also disrupt your sex life, leave you tired and short-tempered, or cause rashes or infection due to the leaks. And the whole experience may leave you feeling unhappy and hopeless.
Strategies for Overcoming Overactive Bladder
The good news is that overactive bladder can be controlled. In fact, many patients overcome OAB without the need for invasive medical and surgical procedures. The key to successful treatment is seeing a urologist early to assess your condition and identify steps to help you manage the symptoms and regain control over your bladder.
Lifestyle measures may include changing what you eat or drink, pelvic floor exercises, and pre-planned bathroom visits. When lifestyle changes are unsuccessful, medical and surgical interventions may be necessary.
Behavioral Changes
1. Reducing fluid intake
Restricting fluid intake reduces your urinary output and helps control OAB symptoms. Since the symptoms of overactive bladder usually occur after a certain critical urinary volume is reached in the bladder, limiting fluid intake ensures it takes longer to reach this critical volume.
By consuming most of your fluid before 7 PM, you can lessen your nocturnal frequency. If you are on diuretic medications, you can check with your urologist to see whether they can be changed.
2. Limiting foods and drinks that trouble your bladder
Alcohol and caffeine (present in coffee, tea, colas, chocolate and some energy drinks) irritate the bladder and increase urinary output. By reducing the intake of these beverages and foods, you can improve your bladder control.
Foods such as fruits and vegetables have hidden water content, so you can limit additional beverages when eating healthy fresh produce. You might also want to reduce or abstain from spicy foods, citrus fruits, and artificial sweeteners, foods made with tomatoes, soda, and other fizzy drinks.
Because the chemical constituents of tobacco constrict blood vessels, impair blood flow, decrease oxygenation, and promote inflammation—affecting the bladder, urethra and pelvic floor muscles—quitting cigarette smoking will improve your OAB symptoms.
3. Keep a bladder diary
Writing down the time and triggers for your trips to the bathroom can help you understand your body better. After a few days, your diary will show you the things that make your symptoms worse. For instance, you may realize that your symptoms get worse after you eat or drink a certain food. This helps you to decide what changes to make in your diet.
4. Weight loss and regular exercise
Excess weight puts pressure on the urinary bladder and worsens overactive bladder. Even modest weight loss may improve your overactive bladder symptoms.
Lower impact exercises, such as yoga, cycling, Pilates, and swimming, can help to alleviate pressure on the urinary bladder by boosting core muscle strength and tone. As a result, OAB symptoms improve.
Due to the proximity of the rectum to the bladder, a full rectum can put pressure on your bladder, resulting in worsening of urgency, frequency and incontinence. Taking steps to avoid constipation will improve bladder control.
Voiding Measures and Bladder Retraining
You can overcome overactive bladder by managing how and when you void. Ways to manage voiding include delayed (inhibited) voiding, timed voiding, and double voiding. Bladder retraining gradually imposes increased intervals between voids and establishes a more normal pattern of urination.
Delayed voiding means you practice waiting before you can go into the bathroom, even when you feel the urge. At the beginning, you may try waiting a few minutes, then gradually increase your waiting time to achieve a delay of up to 2-3 hours.
By timed voiding, you follow a daily pre-planned bathroom schedule. That is, instead of going to the bathroom every time you feel the urge, you go at set times during the day. For example, you may try to pass urine every 2-4 hours regardless of whether you have the urge to go or not. The goal of doing this is to prevent an urgent uncontrollable feeling and to regain control over your bladder.
Double voiding (emptying your bladder twice) helps if you have trouble emptying your bladder. After you go to the bathroom, try again a minute later.
Pelvic Floor Muscle Training
Pelvic floor muscle exercises, also called Kegel exercises, help to stimulate inhibitory reflexes between the bladder and the pelvic floor muscles. By exercising your pelvic floor muscles rhythmically, you can inhibit involuntary contraction before and after it begins.
Kegel exercises target muscles that relax the bladder. To perform the exercises, you should begin by mastering the presence, location, and nature of the pelvic floor muscles. A simple means of identifying the muscles is to start urinating and then, when about halfway completed, to abruptly stop the urine stream.
Once you locate the muscles, squeeze them just before and during the trigger for urgency or incontinence. This will diminish the urgency and help avoid the incontinence. When performing Kegel exercises, always squeeze and relax the muscles repeatedly when you feel the urge to pass urine.
Medications
Bladder relaxant medications can help you suppress overactive bladder symptoms, although you may need several trials of different medications or combinations of medications to achieve optimal results.
Your urologist will prescribe medication either in conjunction with behavioral modification or after behavior modification has been tried unsuccessfully. The drugs prevent involuntary contractions of the bladder muscles by relaxing and stabilizing them.
Biofeedback and Botox injections
Biofeedback is an adjunct to training pelvic floor muscles in which electronic instrumentation is used to transmit feedback information about pelvic floor muscle contractions. It enhances awareness and strength of pelvic floor muscles.
In other cases, your urologist may opt for Botox—a simple procedure usually done in the doctor’s office—where it is injected directly into the bladder muscle to help reduce OAB symptoms. Once injected, Botox helps to relax areas of the bladder where it is injected. Botox injections generally last 6-9 months and are covered by Medicare and most insurance companies.
Percutaneous Tibial Nerve Stimulation (PTNS) and Interstim
PTNS is a minimally invasive form of neuro-modulation. A tiny acupuncture-style needle is inserted near the tibial nerve in the ankle and a hand-held stimulator used to generate electrical stimulation with the intent of improving OAB symptoms. The procedure is performed once every week for 12 weeks.
In some cases, your urologist may opt for the more invasive form of neuro-modulation, called interstim. During the interstim procedure, electrical impulses are used to stimulate and modulate the sacral nerves in the effort to relieve OAB symptoms. A battery-powered neuro-stimulator (bladder “pacemaker”) is used to provide the mild electrical impulses that are carried by a small lead wire to the stimulated sacral nerves affecting bladder function.
Surgery for Overactive Bladder
Treating OAB with surgery is not common and is usually reserved for cases where other treatment plans have failed. Surgery may increase the physical size of the bladder by using portions of the bowel to replace and expand a section of the bladder.
At St Pete Urology, our approach to helping you overcome overactive bladder includes lifestyle changes and medical treatments such as prescription drugs, bladder Botox treatment, nerve stimulation, and surgery. Our specialist team of urologists is experienced at dealing with overactive bladder through proper diagnosis and treatment. You can be sure your consultation will lead to a recommendation of the best possible treatment options for you. Schedule your appointment with us and begin your journey to freedom from overactive bladder. For more information on overcoming overactive bladder and other urologic conditions, visit the St Pete Urology website.
What Causes Low Sperm Count?
 Low sperm count, which means having fewer than normal sperm in the ejaculate, decreases the likelihood that your sperm will fertilize your partner’s ovum and result in pregnancy. But it may also be related to your overall health, as it is often characterized by symptoms such as pain, swelling or a lump in the testicle area, low sex drive, erectile dysfunction, or decreased facial or body hair. Your sperm count is lower than normal if you have fewer than 15 million sperm per milliliter of semen.
Low sperm count, which means having fewer than normal sperm in the ejaculate, decreases the likelihood that your sperm will fertilize your partner’s ovum and result in pregnancy. But it may also be related to your overall health, as it is often characterized by symptoms such as pain, swelling or a lump in the testicle area, low sex drive, erectile dysfunction, or decreased facial or body hair. Your sperm count is lower than normal if you have fewer than 15 million sperm per milliliter of semen.
What are the causes of low sperm count?
1. Emotional stress and inadequate sleep
Prolonged or severe emotional stress may interfere with the hormones needed to produce sperm, while depression lowers sperm concentration. Inadequate sleep makes it difficult to maintain a healthy weight and may lead to obesity. Obesity impairs fertility by directly impacting sperm and causing changes in the hormones that promote sperm production.
2. Overexposure to harmful chemicals
Chronic exposure to pesticides and other harmful chemicals can lead to low sperm count. For instance, prolonged exposure to industrial chemicals, such as xylene, toluene, benzene, herbicides, pesticides, organic solvents, BPA, perfluorinated chemicals, lead, and painting materials may lead to low sperm count. Likewise, when exposure to radiation or x-rays lowers sperm production, it can take years for sperm production to normalize.
3. Lack of exercise
Exercise plays a huge role in the health of your sperm. Men who sit for longer periods tend to have a lower sperm count than those who are active in their daily life. This means you can improve your numbers through moderate routine exercise every day, such as a daily walk for lunch or daily yoga in the evenings. Frequent exercise will increase your circulation, boost your mood, and increase your sperm count.
4. Overheating of the testicles
Exposure to high temperatures impairs sperm production and function. This is why frequent use of hot tubs or saunas temporarily lowers sperm count. Similarly, wearing tight clothing, sitting for long periods or working on a laptop for a long period of time may raise the temperature around the scrotum and reduce sperm production.
5. Drug and alcohol use
Anabolic steroids that are taken to stimulate muscle growth and can cause testicular shrinkage and decreased sperm production. Use of cocaine or marijuana also lowers sperm number and quality, while excessive drinking of alcohol lowers testosterone levels and hampers sperm production. Men who smoke tend to have a lower sperm count than those who do not.
6. Infection, medications and prior surgery
Some infections interfere with sperm production and sperm health. They include epididymitis (inflammation of epididymis), orchitis (inflammation of testicles), sexually transmitted infections (like gonorrhea, Chlamydia and HIV), and mumps infection. Also, long-term anabolic steroid use, cancer medications, testosterone replacement therapy, some ulcer medications, some antifungal and antibiotic medications, and other medications can hinder sperm production and lower sperm count.
Prior surgeries such as a vasectomy, scrotal or testicular surgery, inguinal hernia repair, prostate surgery, and large abdominal surgery for testicular or rectal cancer may affect sperm production. Similarly, tubes that carry sperm may be blocked by injury from surgery, trauma, prior infections, or abnormal development such as cystic fibrosis. Spinal cord injuries, diabetes and surgeries can block the normal flow of sperm and lead to retrograde (backward) ejaculation.
7. Certain medical conditions
A varicocele, the swelling of veins that drain the testicle, impairs testicular temperature regulation and causes low sperm count. Anti-sperm antibodies, which are immune cells that mistakenly identify sperm as harmful invaders, may destroy sperm and lead to low sperm count.
Undescended testicles, Peyronie’s disease, sperm duct problems, vas deferens blockages, unhealthy prostate, high blood pressure, diabetes, peripheral vascular disease, tumors that affect male reproductive organs directly, and hormonal imbalances may impair sperm production and lower sperm count.
What should you do to improve your sperm count?
- Eat healthy
- Exercise regularly and minimize your sitting time
- Don’t smoke
- Reduce or abstain from alcohol
- Avoid illicit drugs
- Use protection (condoms) during sexual intercourse
- Manage stress
- Get enough sleep
- Maintain a healthy weight
- Avoid exposure to pesticides, heavy metals, and other toxins
- Keep your laptop away from your lap
- Speak with your doctor about medications that can affect your sperm count
- Avoid frequent hot showers or hot tubs.
- Avoid tight pants
Maintaining a high sperm count is not necessarily difficult. All you need is some good habits such as healthy eating, regular exercise, comfortable clothes, and avoiding toxins. You should also speak with your urologist about possible remedies.
At St Pete Urology, we offer a variety of treatments for low sperm count, including lifestyle changes and minimally invasive procedures. We make sure to conduct thorough physical exams, medical history, and diagnostic tests to establish the underlying cause of the low sperm count before we recommend treatment. Meet with one of our urologists and start your journey to healthy fertility. For more information on male fertility, erectile dysfunction and other urologic issues, visit the St Pete Urology website.
How and Why Should I Do Kegels?
 Kegel exercises are for strengthening pelvic floor muscles. They involve contracting and relaxing, clenching and releasing those muscles. Also called pelvic floor exercises, Kegels strengthen and coordinate the muscles that support the bladder, rectum, uterus and small intestines. The strengthening, in turn, helps to prevent the accidental passing of stool or gas, stops bladder leaks, and improves orgasm.
Kegel exercises are for strengthening pelvic floor muscles. They involve contracting and relaxing, clenching and releasing those muscles. Also called pelvic floor exercises, Kegels strengthen and coordinate the muscles that support the bladder, rectum, uterus and small intestines. The strengthening, in turn, helps to prevent the accidental passing of stool or gas, stops bladder leaks, and improves orgasm.
What are the benefits of Kegel exercises?
1. Prevent pelvic organ prolapse
Pelvic floor muscles support abdominal organs such as the stomach, bladder, intestines and uterus. With age, the weakening and slowing down of these muscles may lead to pelvic organ prolapse (POP).
A prolapse means the pelvic organs are displaced, drooping and fallen out of their normal position. In women, the pelvic organs may fall into the vagina or cause vaginal tissues to protrude from the body, particularly if the prolapse occurs after a hysterectomy.
Through regular Kegel exercises, pelvic floor muscles become stronger and more coordinated, reducing the risk of prolapse.
2. Avert incontinence
Pelvic floor exercises not only contribute to good posture and spinal stability, they also strengthen the muscular support for bladder and bowel function and help to maintain urinary and fecal continence. If you already have bowel or bladder incontinence, or drip after peeing, the exercises can help to relieve your symptoms.
3. Enhance sexual function
Kegel exercises improve sexual function. In men, they increase control over ejaculation and enhance the feeling experienced during orgasm. In women, the exercises improve flexibility and ease penetration. In addition, they provide the muscular strength to achieve orgasm while also making pregnancy and childbirth easier.
How should you do Kegel exercises?
1. Begin by identifying pelvic floor muscles
Kegel exercises do not require a lot of time, but targeting the right muscles is necessary. One of the easiest ways to identify the muscles is to stop urinating midstream by squeezing your muscles to hold the urine in. Another way of locating the muscles is to stop the passage of gas.
The muscles that help you to stop the passage of urine or gas are the ones you will need to work on. You only need to stop passing urine once or twice in order to identify the right muscles. After that, it is not advisable to perform Kegel exercises while urinating as that can lead to incomplete emptying of the bladder and increased risk of urinary tract infections.
2. Start slowly and improve with practice
Like other exercises, Kegels become easier with practice. Plan to begin slowly and build on your gains over time. For instance, you can start by squeezing your pelvic floor muscles for 3 seconds, releasing for another 3 seconds, and then repeating 10 times in a row. If you are not able to do 10 at time, begin with a lower number and increase with time.
3. Keep the focus
As you do these exercises, you will be tempted to flex the buttocks, thighs or abdomen. You may also find it difficult to increase the number of repetitions. Always target and exercise your pelvic floor muscles, pushing your body to complete at least one set of 10 Kegel exercises two to three times a day.
As you do the exercises, make sure to relax your pelvic floor muscles completely and to avoid holding your breath.
4. Perform Kegels anytime, anywhere
Kegel exercises are quite convenient. You can make them part of your routine and do them anywhere, whether brushing your teeth, driving to work, shopping for groceries or watching TV. Combining the exercise with another activity is a good way to remember your routine and see quick results.
Can Kegel exercises cause complications?
While the exercises are completely safe, you still need to do them the right way. For instance, you should not overdo Kegels as this may lead to straining when you visit the bathroom. You should also not do them as you urinate because that could increase your risk of urinary tract infections.
Kegel exercises are not for everyone. If your muscles are already tired, they will not respond if you try to contract them. Also, if your muscles are already tight, exercising them may cause more harm. Speak with your urologist to determine if you can benefit.
Are the exercises effective?
For those who do Kegel exercises regularly, the results are excellent. For example, urine leaks become less frequent within a few weeks of starting the exercises. Keep in mind that they have more impact when performed regularly over an extended period of time, such as doing them every day for at least 15 weeks. If you do not feel your symptoms are improving, you should speak with your doctor about alternative treatments.
At St Pete Urology, we offer personalized treatments for patients with urological problems. We will only recommend you do Kegel exercises after a thorough assessment of your condition. For more information on pelvic floor exercises and other treatment options for urologic disorders, visit the St Pete Urology website.

 There is no such thing as “normal” when it comes to sex. What you like isn’t necessarily what another person likes. How important it is to you and how often you want it is also a personal preference, but what is common for everyone is the desire to have a pleasurable sexual encounter.
There is no such thing as “normal” when it comes to sex. What you like isn’t necessarily what another person likes. How important it is to you and how often you want it is also a personal preference, but what is common for everyone is the desire to have a pleasurable sexual encounter.