Testosterone hormone therapy comes in three different forms; intramuscular injection, patch, or gel form. The injection is usually administered once a week, the patch and gel are both placed on the skin as directed by the doctor [Read Full Article…]
Urology Patient Testimonial
Dr. Graves is the kindest, most thoughtful, genuinely caring doctor I have ever encountered in my entire life; and my brother had cancer when we were three and mom had a triple by-pass at twelve. I grew up in hospitals, but I have not spent much time in them for myself since very recently. I would rather pass a stone at home-and have twice- than have the kidney stone blasted at the hospital because of the pain afterward from endometriosis. Dr Graves called me HIMSELF to check on me. Choose him. – Kendra Burke
Directions to St Pete Urology
St Pete Urology is conveniently located at 830 Central Ave, Suite 100 St. Petersburg, Florida 33701 USA [Read Full Article…]
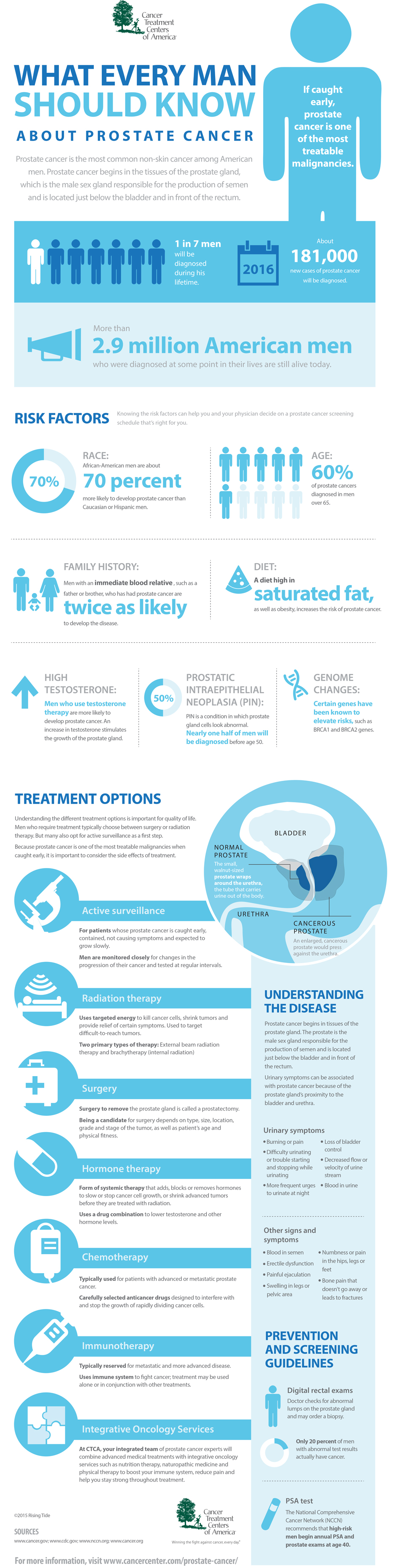
Prostate cancer Infographics
Prostate cancer is the most common non-skin cancer among American men. Every year, 1 in 7 men will be diagnosed with the disease. But prostate cancer is one of the most treatable malignancies, if caught early.
What is Voiding Dysfunction? Treating it Using a Minimally Invasive Procedure
Voiding Dysfunction is a general term to describe the condition where there is a lack of coordination between the bladder muscle (detrusor) and the urethra. [Read Full Article…]
Are certain foods helpful in addressing erectile dysfunction (ED)?
 It’s possible. Research published in January 2016 found that men who ate foods high in antioxidants called flavonoids had a lower risk of erectile dysfunction (ED) than those who didn’t eat a flavonoid-rich diet.
It’s possible. Research published in January 2016 found that men who ate foods high in antioxidants called flavonoids had a lower risk of erectile dysfunction (ED) than those who didn’t eat a flavonoid-rich diet.
Flavonoids can be found in certain plant-based foods like citrus fruits, blueberries, strawberries, apples, pears, cherries, blackberries, radishes, and blackcurrant. Some teas, herbs, and wines also have flavonoids in them.
Past studies have shown that consuming flavonoids could reduce a person’s risk for diabetes and heart disease, both of which can lead to ED.
Eating a healthy diet overall, particularly a Mediterranean diet, can go a long way in preserving erectile function, however.
This type of diet includes fruits, vegetables, whole grains, and olive oil. Nuts and fish are good additions.
What does diet have to do with erections?
When a man is sexually-aroused, his penis fills with blood, giving it the firmness it needs for sex. Many men with ED have poor blood flow to the penis. Some medical conditions, like diabetes and heart disease, can damage blood vessels and nerves that are critical for this process.
Eating a healthy diet keeps the body in good working order. It can help men maintain a healthy weight, keep their blood sugar under control, and reduce the risk of blood vessel damage, which can impair blood flow.
Diet isn’t the only path to good erections, however. Other lifestyle habits, like regular exercise, quitting smoking, and managing depression are important too.
A man’s doctor can help him decide which dietary changes to make. However, men who are having trouble with erections should be sure to mention it. Many factors can contribute to ED and it’s best to have a complete medical checkup. [Read Full Article…]
The Prostate Cancer Test That Saved My Life
“Yeah,” he said, in a slightly nonplussed way, gazing at the results, “I was surprised myself.”
As my new, world-altering doctor spoke about cell cores and Gleason scores, probabilities of survival, incontinence and impotence, why surgery would be good and what kind would make the most sense, his voice literally faded out like every movie or TV show about a guy being told he had cancer… a classic Walter White moment, except I was me, and no one was filming anything at all.
 I got diagnosed with prostate cancer Friday, June 13th, 2014. On September 17th of that year I got a test back telling me I was cancer free. The three months in between were a crazy roller coaster ride with which about 180,000 men a year in America can identify.
I got diagnosed with prostate cancer Friday, June 13th, 2014. On September 17th of that year I got a test back telling me I was cancer free. The three months in between were a crazy roller coaster ride with which about 180,000 men a year in America can identify.
Right after I got the news, still trying to process the key words echoing dimly in my head (probability of survival–vival-vival-val…” “incontinence-nence-nence-ence …), I promptly got on my computer and Googled “Men who had prostate cancer.” I had no idea what to do and needed to see some proof this was not the end of the world.
John Kerry… Joe Torre… excellent, both still going strong. Mandy Patinkin… Robert DeNiro. They’re vital. OK great. Feeling relatively optimistic, I then of course had to do one more search, going dark and quickly tapping in “died of” in place of “had” in the search window.
As I learned more about my disease (one of the key learnings is not to Google “people who died of prostate cancer” immediately after being diagnosed with prostate cancer), I was able to wrap my head around the fact that I was incredibly fortunate. Fortunate because my cancer was detected early enough to treat. And also because my internist gave me a test he didn’t have to.
Taking the PSA test saved my life. Literally. That’s why I am writing this now. There has been a lot of controversy over the test in the last few years. Articles and op-eds on whether it is safe, studies that seem to be interpreted in many different ways, and debates about whether men should take it all. I am not offering a scientific point of view here, just a personal one, based on my experience. The bottom line for me: I was lucky enough to have a doctor who gave me what they call a “baseline” PSA test when I was about 46. I have no history of prostate cancer in my family and I am not in the high-risk group, being neither — to the best of my knowledge — of African or Scandinavian ancestry. I had no symptoms.
What I had — and I’m healthy today because of it — was a thoughtful internist who felt like I was around the age to start checking my PSA level, and discussed it with me.
If he had waited, as the American Cancer Society recommends, until I was 50, I would not have known I had a growing tumor until two years after I got treated. If he had followed the US Preventive Services Task Force guidelines, I would have never gotten tested at all, and not have known I had cancer until it was way too late to treat successfully.
Now, in my case, my doctor, Bernard Kruger, watched my PSA tests rise for over a year and a half, testing me every six months. As the numbers continued to rise, he sent me to the urologist, who gave me a slightly invasive physical check in his office using a gloved finger. This took all of 10 seconds. While I don’t recommend it for fun, amazingly some don’t recommend it at all. After this exam, and looking at my rising PSA numbers, he suggested an MRI to get a roadmap of my prostate.
It’s a non-invasive procedure like the one athletes get to check for torn ACLs. Loud, but painless. Only after studying the MRI results did my doctor recommend a not-fun-at-all biopsy. Unlike the MRI, the biopsy was as invasive as it gets: long needles in sensitive places and more small talk about kids and school pick ups while it was all going down.
Then the biopsy came back positive. Of course “positive” for medical tests is usually not so positive. I had a Gleason score of 7 (3+4), which is categorized “mid-range aggressive cancer.” Surgery was recommended. At this point I decided to go out and get a few different opinions. All the doctors I talked to concurred that the tumor needed to be taken out.
Ultimately, I found a wonderful surgeon named Edward Schaeffer who I felt comfortable with. He performed a robotic assisted laparoscopic radical prostatectomy. Due to a lot of skill and a little beneficence from some higher power, he got all the cancer. As of this writing I am two years cancer free and extremely grateful.
So. What is the deal with this PSA test and why the controversy?
It is a simple, painless blood test. It is not dangerous in itself in any way. If the PSA (Prostate Specific Antigen) value is elevated in the blood, or levels rise sharply over time, it could indicate the presence of prostate cancer. It is definitely not foolproof.
The criticism of the test is that depending on how they interpret the data, doctors can send patients for further tests like the MRI and the more invasive biopsy, when not needed. Physicians can find low-risk cancers that are not life threatening, especially to older patients. In some cases, men with this type of cancer get “over-treatment” like radiation or surgery, resulting in side effects such as impotence or incontinence. Obviously this is not good; however it’s all in the purview of the doctor treating the patient.
But without this PSA test itself, or any screening procedure at all, how are doctors going to detect asymptomatic cases like mine, before the cancer has spread and metastasized throughout one’s body rendering it incurable? Or what about the men who are most at risk, those of African ancestry, and men who have a history of prostate cancer in their family? Should we, as the USPSTF suggests, not screen them at all? There is growing evidence that these guidelines have led to increased cases of prostate cancers that get detected too late for the patient to survive the disease.
Five years after their initial recommendation to stop PSA testing, the USPSTF is presently, per their website, “updating their recommendations.” I think men over the age of 40 should have the opportunity to discuss the test with their doctor and learn about it, so they can have the chance to be screened. After that an informed patient can make responsible choices as to how to proceed.
I count my blessings that I had a doctor who presented me with these options. After I chose to take the test, he directed me to doctors who worked at centers of excellence in this field to determine the next steps. This is a complicated issue, and an evolving one. But in this imperfect world, I believe the best way to determine a course of action for the most treatable, yet deadly cancer, is to detect it early.
What Everyone Should Know About Retrograde Ejaculation
Retrograde ejaculation happens when semen enters the urinary bladder during ejaculation instead of moving out through the urethra. It may be caused by diabetes (32% of men with diabetes mellitus have this condition), nerve problems, or surgery of the urethra or prostate. Some medications used for treating high blood pressure, mood disorders and benign prostate hyperplasia are also known to cause this problem.
Symptoms
- Little or no semen is secreted during ejaculation, a condition referred to as a dry orgasm.
- After an orgasm, the urine looks cloudy due to the presence of semen.
- Infertility is common in men with this problem.
Tests to Detect Retrograde Ejaculation
First, the genitals are physically examined for any anatomical defects. Following an exam, a “urinalysis” lab test of a urine sample collected immediately after ejaculation indicates the amount of sperm in the urine.
Treatment Options
In most cases, the diagnosis is carried out by a urologist specializing in urinary tract disorders and male reproductive problems, and the treatment procedure varies depending on the cause of the condition. If retrograde ejaculation occurs as a side effect of medication, discontinuing that medication usually resolves the problem. In cases where retrograde ejaculation occurs as a result of spinal cord injury, genitourinary tract surgery, or nerve damage caused by diabetes mellitus, epinephrine-like drugs are known to help, but the condition may not be completely curable. Although surgery is available, it is rarely a primary treatment for this condition since the results are found to be inconsistent.
Prevention
Diabetic men with this ejaculatory disorder are advised to keep their blood sugar levels under control. Also, diabetics and men with reproductive disorders should avoid medication that is known to cause retrograde ejaculation. If you notice a trace of cloudiness in your urine, you should make an appointment with a urologist right away because the treatments for retrograde ejaculation are more effective when the condition is detected early.
The Penile Prosthesis Procedure
Penile Prosthesis devices are either malleable (bendable) or inflatable. The simplest consists of a pair of malleable rods surgically implanted within the erection chambers of the penis [Read Full Article…]
What is UroLift System? – Treatment for BPH (Enlarged Prostate)
Patients with an enlarged prostate can benefit greatly from treatment and care options available in urology clinics. A urologist will examine the patient and assess the severity of the symptoms before prescribing any treatment. [Read Full Article…]